thomas jefferson university
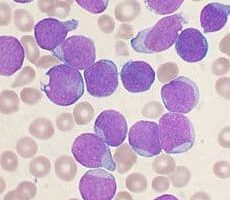
Disease progression halted in rat model of Lou Gehrig’s disease
Amyotrophic lateral sclerosis (ALS; also known as Lou Gehrig’s disease) is an incurable adult neurodegenerative disorder that progresses to paralysis and death. Genetic mutations are the cause of disease in 5% of patients with ALS. Of immense interest,…
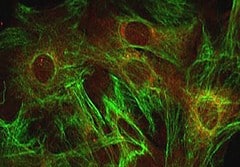
Nature study: Jefferson researchers unravel protein’s elusive role in embryo and disease development
PHILADELPHIA — Reporting in Nature, scientists from Thomas Jefferson University have determined that a single protein called FADD controls multiple cell death pathways, a discovery that could lead to better, more targeted autoimmune disease and can…
Drug that helps adults addicted to opioid drugs also relieves withdrawal symptoms in newborns
(PHILADELPHIA) – Thousands of infants each year have exposure to opioids before they are born. Over half of these infants are born with withdrawal symptoms severe enough to require opioid replacement treatment in the nursery. Such treatment is assoc…
Researchers nationwide ask for new focus on ‘sudden death’ heart disorder
(PHILADELPHIA) An abrupt, fatal heart attack in a young athlete on the playing field is a tragedy destined to repeat itself over and over until more is understood about hypertrophic cardiomyopathy (HCM), a genetic disorder that is the most common ca…
Breathing Device May Help Spare Tissue from Radiation Side Effects
A special breathing technology may help spare healthy lung, heart and liver tissue from the effects of radiation during treatment for early stage breast cancer. Kolby Sidhu, M.D., an instructor in radiation oncology at Jefferson Medical College of Thomas Jefferson University in Philadelphia, leads a clinical trial examining the effectiveness of the Active Breathing Coordinator (ABC), a device that is aimed at helping patients to hold their breath in a consistent manner while receiving radiation. This inhalation in turn increases the separation between the breast tissue and the heart, reducing the heart’s exposure to radiation during treatment.
Light therapy may help treat advanced lung cancer
Surgeons in Philadelphia say they are finding success by combining light-based cancer therapy with surgery to treat patients with advanced lung cancer that has spread within the chest. While the number of patients treated to date is small, many patients are living three to four times longer than did those patients who did not receive the therapy. In photodynamic therapy (PDT), a nontoxic photosensitizing agent, photofrin, is injected into the bloodstream and absorbed by cells all over the body. These compounds tend to concentrate more in cancer cells than in normal cells. When the compound is exposed to a certain wavelength of light, it absorbs the light energy and produces a form of oxygen that kills the cells. The damage occurs only where the light is shined. In the study, each patient is given chemotherapy until the cancer stops responding, meaning the disease begins to grow again. If the cancer has not spread beyond the chest, the patient then receives photofrin 24 hours prior to surgery to remove the tumor. During surgery, he or she receives an appropriate dose of light therapy. Of the 16 patients evaluated to date, at least one-half have lived more than 23 months, which is between three and four times the usual time.
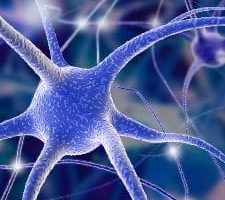
Human Neural Stem Cells Can Become Dopamine-Making Brain Cells
Biologists have shown for the first time in the laboratory that they can convert some adult human neural stem cells to brain cells that can produce dopamine, the brain chemical missing in Parkinson’s disease. If the researchers can better understand the process and harness this ability, the work may someday lead to new strategies in treating neurodegenerative diseases such as Parkinson’s.
Teen brain more sensitive to addictive drugs
Researchers have found evidence in animals that the young, adolescent brain may be more sensitive to addictive drugs such as cocaine and amphetamines than either the adult or newborn. The work may help someday lead to a better understanding of how the adolescent human brain adapts to such drugs, and provide clues into changes in the brain that occur during drug addiction.
Parkinson’s patients look to gene therapy