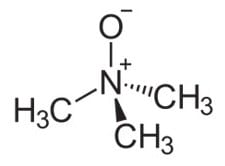
In the last five years, some scientists have cautioned against eating eggs and meat because these foods generate a common dietary compound, trimethylamine N-oxide (TMAO), that research has suggested plays a role in heart disease.
A Cornell study recently published online in the peer-reviewed journal Molecular Nutrition and Food Research reports new results that raise questions about whether circulating TMAO causes heart disease or whether it is simply a biomarker, or a sign, of developing disease.
TMAO is naturally found in fish at high levels. In humans, gut bacteria called firmicutes help convert the nutrient choline (from eggs) and carnitine (from meat) into TMAO.
In the study, the researchers found that healthy men with elevated TMAO levels after eating eggs and beef also had high counts of firmicutes.
“The findings demonstrate that a person’s gut microbiome can influence circulating TMAO,” said Marie Caudill, Cornell professor of nutritional sciences and the paper’s senior author. “It also raises questions about the causative role of TMAO in the disease process, and it begs the question whether the gut microbiome is playing a role in the disease process rather than the TMAO itself.”
In 2011, other researchers looked at blood profiles in people with cardiovascular disease and found high levels of circulating TMAO. Follow-up studies implicated TMAO in the formation of arterial plaque in mice. Also, previous research has shown that women who developed colon cancer had elevated TMAO five years prior to the onset of their cancers.
These results led some researchers to recommend people avoid eating fish, eggs and meat, Caudill said.
“We questioned how TMAO could be a causative agent of heart disease given decades of research showing that high fish consumption lowered risk of heart disease,” she said.
In the current study, Caudill and colleagues conducted feeding trials where 40 healthy young men consumed four different study meals: one of fish (6 ounces of cod), one of eggs (three whole hard boiled eggs), one of meat (6 ounces of beef patty) and one of fruit (apple sauce) as a control. Each of these meals was administered in random order in a single day separated by a one-week washout period. Before each meal, feces were collected to profile gut microbiota compositions, and blood and urine were collected to measure TMAO levels. Blood and urine were also collected for TMAO measurements in intervals of up to six hours following each meal.
Men with elevated TMAO levels after eating meals of eggs and beef were found to have higher levels of firmicute bacteria in their guts, while those with lower levels of TMAO had higher levels of a class of bacteria called bacteriodides. Firmicutes alone express genes that convert choline (from eggs) and carnitine (from beef) to TMA, which the body in turn converts to TMAO. Those with high TMAO also had less-diverse gut microbiomes.
When these men ate fish, circulating TMAO increased within 15 minutes by 50 times compared with measurements after eating eggs or beef. But, in the U.S., fish is generally not a major part of diets, while Americans eat a lot of eggs and meat, Caudill said.
“This provides some evidence that the elevation in TMAO may simply be a biomarker of differences in the gut microbiome,” Caudill said. “My hypothesis is that diseased individuals – whether it’s heart disease, cancer or other chronic diseases – are going to have a different microbiome than nondiseased individuals, and that microbiome can be marked by TMAO levels in the blood.”
Future research may include testing the role of gut microbiomes in heart disease, and looking at ways to reduce circulating TMAO and seeing if there are benefits that reduce heart disease, Caudill said.