A type of treatment for multiple sclerosis that ‘resets’ the immune system may stop progression of the disease in nearly half of patients.
In a new study, led by Imperial College London, the treatment prevented symptoms of severe disease from worsening for five years, in 46 per cent of patients.
However, as the treatment involves aggressive chemotherapy, the researchers stress the procedure carries significant risk.
Multiple sclerosis (MS) affects around 100,000 people in the UK, and 2.3 million worldwide. The condition is caused by the immune system malfunctioning and mistakenly attacking nerves in the brain and spinal cord. This leads to a range of symptoms including fatigue, problems with arm and leg movement, vision and balance. There is no cure but certain medications can help slow progression of the disease.
The treatment in the current study, called autologous hematopoietic stem cell transplantation (AHSCT), was given to patients with advanced forms of the disease that had failed to respond to other medications.
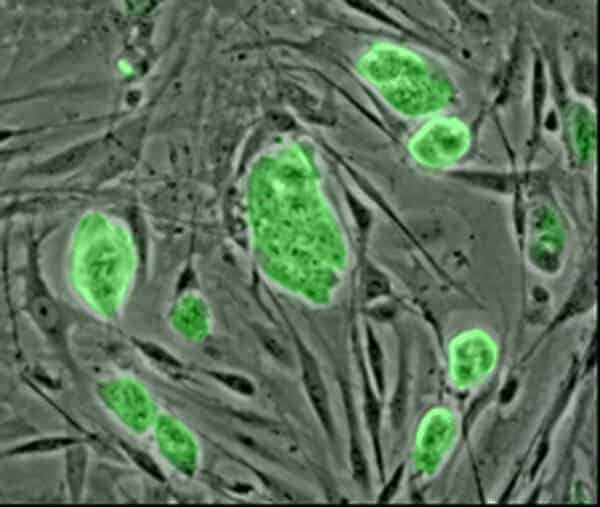
The study, published in the journal JAMA Neurology, suggested some patients even saw a small improvement in their symptoms following the treatment. The one-off treatment aims to prevent the immune system from attacking the nerve cells. All immune system cells are made from stem cells in the bone marrow. In the treatment, a patient is given a drug that encourages stem cells to move from the bone marrow into the blood stream, and these cells are then removed from the body.
The patient then receives high-dose chemotherapy that kills any remaining immune cells. The patient’s stem cells are then transfused back into their body to re-grow their immune system. Previous studies have suggested this ‘resets’ the immune system, and stops it from attacking the nerve cells.
However, because the treatment involves aggressive chemotherapy that inactivates the immune system for a short period of time, some patients died from infections. Out of the 281 patients who received the treatment in the study, eight died in the 100 days following the treatment. Older patients, and those with the most severe forms of the disease, were found to have a higher risk of death.
Dr Paolo Muraro, lead author of the study from the Department of Medicine at Imperial, explained that the risks must be weighed-up against the benefits: “We previously knew this treatment reboots or resets the immune system – and that it carried risks – but we didn’t know how long the benefits lasted.
“In this study, which is the largest long-term follow-up study of this procedure, we’ve shown we can ‘freeze’ a patient’s disease – and stop it from becoming worse, for up to five years.
However, we must take into account that the treatment carries a small risk of death, and this is a disease that is not immediately life-threatening.”
Most patients with multiple sclerosis have a type of the disease that has flare-ups, known as relapses, followed by an improvement in symptoms. This is called relapsing-remitting MS.
Dr Muraro explained the number of years this treatment prevented symptoms from worsening is far greater than would be expected in untreated patients with severe forms of relapsing MS.
The study found that in patients with relapsing MS, nearly three in four (73 per cent) experienced no worsening of their symptoms five years after the treatment. Younger patients with less severe forms of the disease were more likely respond to the therapy.
However, the majority of the patients in the study had a progressive form of MS. This is a more severe form of the disease, and for which there are currently no treatments. Among these patients, one in three experienced no worsening of symptoms five years after treatment.
Some patients saw a small improvement in their symptoms, though this improvement was larger in patients with relapsing MS, compared to patients with the progressive form.
Disability in MS is assessed on a scale known as the Expanded Disability Status Scale (EDSS). In this scale, zero represents no disability, seven is wheelchair-bound, while ten is death from MS. At the beginning of the study, patients had an average EDSS score of 6.5.
Patients with relapsing MS had an average improvement in their EDSS score of 0.76, one year after the treatment. Patients with progressive MS had only a marginal improvement of 0.14.
Dr Muraro added these findings suggest larger trials of this procedure are now needed.
“These findings are very promising – but crucially we didn’t have a placebo group in this study, of patients who didn’t receive the treatment. We urgently need more effective treatments for this devastating condition, and so a large randomised controlled trial of this treatment should be the next step.”
Dr Sorrel Bickley, Head of Biomedical Research at the MS Society, added: “This study is one of the largest to date looking at AHSCT as a treatment for MS and the findings offer some encouraging insights. It shows that AHSCT can slow or stop progression for many years, and the treatment is most effective in people with MS who have ‘active inflammation’ in their brain and spinal cord.
“There are more than 100,000 people with MS in the UK, it’s a challenging and unpredictable condition to live with and that’s why the MS Society is funding research like this to further our knowledge and find treatments for everyone.
“If anyone with MS is considering AHSCT they should speak to their neurologist as a referral is needed to access this treatment via a trial or on the NHS.”