Healthy human skin is alive with bacteria. In fact, there are more microorganisms living in and on the human body than there are human cells. Most can live on the human skin without harming the host, but in some people bacteria can negatively alter their health, maybe even become life-threatening.
University of California San Diego School of Medicine researchers screened 10,000 colonies of bacteria found on the epidermis to determine how many had antimicrobial properties and at what rate these are found on healthy and non-healthy skin. In a paper published February 22 in Science Translation Medicine, the team reports isolating and growing good bacteria that produce antimicrobial peptides and successfully transplanting it to treat patients with the most common type of eczema, known as atopic dermatitis.
“We discovered antimicrobial peptides produced by bacteria commonly found on healthy human skin. These novel antimicrobials have selective activity against pathogenic bacteria, but do not harm other commensal bacteria that have a beneficial effect to us,” said Teruaki Nakatsuji, PhD, project scientist in the Department of Dermatology at UC San Diego School of Medicine and first author.
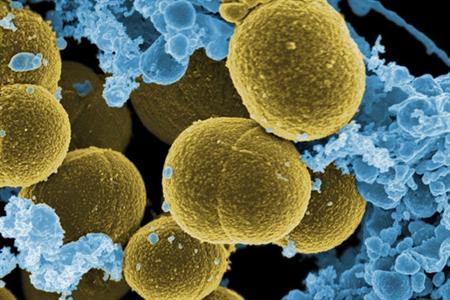
The team tested if bacteria normally found on human skin, including Staphylococcus hominis and Staphylococcus epidermis, defend against Staphylococcus aureus — a pathogenic bacteria that aggravates skin conditions like atopic dermatitis. When S. aureus becomes antibiotic resistant it is known as methicillin-resistant Staphylococcus aureus or MRSA. It is a leading cause of death resulting from infection in the United States.
“We discovered that healthy people have many bacteria producing previously undiscovered antimicrobial peptides, but when you look at the skin of people with atopic dermatitis, their bacteria are not doing the same thing. They have the wrong type of bacteria,” said Richard Gallo, MD, PhD, professor and chair of the Department of Dermatology at UC San Diego School of Medicine. “After isolating the good bacteria and growing it, we were able to transplant it back to people who were deficient in it and it had an immediate impact by reducing the amount of S. aureus on the skin.”
According to the National Eczema Association, nearly 18 million people in the United States are plagued with atopic dermatitis, the most common form of eczema, which normally appears as a rash on arms, legs and cheeks.
The first tests were done in animal models where S. aureus was eliminated by transplanting good bacteria to the area where S. aureus was found. Success with these models led to a small phase I clinical trial in which an individual’s good bacteria with antimicrobial activity was grown, formulated in a skin cream and applied once to the forearm of the eczema patient infected by S. aureus. The phase I trial was intended only to test for safety and efficacy, but every patient treated in this way exhibited a significant decrease in S. aureus on their skin.
“We now have a rational therapeutic approach for atopic dermatitis by using bacterial transplant technology,” said Gallo. “It appears that people with this disorder will need to have it reapplied because their body does not naturally promote the growth of these organisms. The good thing is this is easy to do because it’s just a cream.”
A phase II clinical trial is just beginning to evaluate whether prolonged application of one of the most potent good bacteria from human skin can provide long-term protection against S. aureus and improve atopic dermatitis.
“Using a natural antibiotic produced by the skin microbiome is superior to current pharmaceutical approaches because the bacteriotherapy does not kill protective bacteria strains,” said Nakatsuji. “Antibiotic resistance is not likely to occur because the bacteria therapy is attacking pathogens by multiple different ways at once.”
According to researchers, the microbiome is clearly associated with disease but cause and effect had not been established. This study reveals one of the chemicals that normal skin bacteria make to help humans fight off infection or an imbalance in the skin microflora.