One of the biggest challenges facing medical researchers is that experimental models cannot perfectly replicate human diseases in the laboratory.
That’s why human organs-on-chips have been swiftly adopted by scientists in academic and industry labs and are being tested by the U.S. Food and Drug Administration.
These small devices—developed by bioengineer Donald Ingber, the Judah Folkman Professor of Vascular Biology at Harvard Medical School and Boston Children’s Hospital and director of the Wyss Institute for Biologically Inspired Engineering at Harvard University—mimic human organ environments in an affordable and lifelike manner.
Now, Ingber’s team has developed a lung cancer-on-a-chip platform and discovered an important link between breathing mechanics and lung cancer behavior.
As reported Oct. 10 in Cell Reports, the team leveraged two chips representing different parts of the lung and then grew a common form of lung cancer inside them.
The findings illuminate how the mechanical forces of breathing might encourage the growth of “persister” cancer cells, which linger after treatment and become resistant to drugs, eventually spreading and causing metastasis.
The lung cancer chips “offer a literal window on the biological tumor complexities,” said Ingber, the study’s senior author.
Unraveling the complexities of lung cancer
Organs-on-chips are about the size of a computer memory stick and made of clear polymer. They are called microfluidic devices because they contain hollow channels that are perfused with a lifelike flow of blood substitute, nutrients and cells to mimic the microenvironment of human organs.
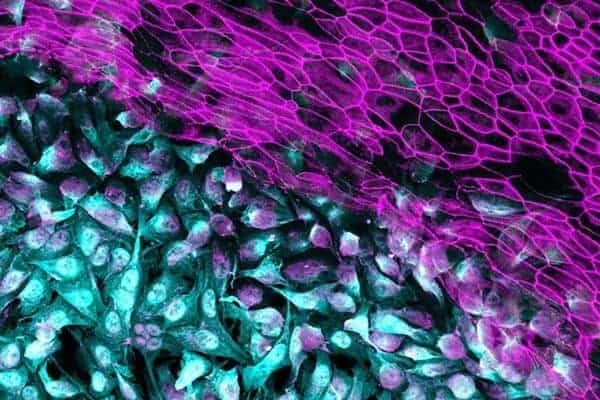
The two lung cancer chips—one of which mimics the small airways of the lung and the second of which mimics the lung’s air sacs, or alveoli, responsible for oxygen and carbon dioxide exchange—were seeded with human adenocarcinoma cells, the most common variety of non-small cell lung cancer.
Inside the chips, the lung cancer cells behaved just like they have been known to do in human patients. In the lung airway chip, the cancer cells first remained dormant before they started to proliferate. In the alveolus-on-a-chip, they proliferated much more aggressively without any lag time.
“This approach allows us to recreate key hallmarks of this cancer, including its growth and invasion patterns, and to determine how they are influenced by cues from surrounding normal cells,” said first author Bryan Hassell, who developed the lung cancer-on-a-chip platform as a graduate researcher on Ingber’s team.
By applying cyclical mechanical forces to the alveolus chips to mimic breathing motions, the researchers noticed that cancer cell growth and invasion were both inhibited.
In human patients, they speculate that as lung cancer cells grow and fill the lung air sacs, the tumor mass interferes with the lung’s natural movements. In turn, this disruption could speed up tumor growth and facilitate invasive behavior leading to metastasis.
Does breathing help lung cancer cells thrive?
Along this line of thinking, Ingber’s team wondered if breathing mechanics could also make lung cancer cells more sensitive to anti-cancer drugs known as TKIs (tyrosine kinase inhibitors), which target mutated enzymes that enable cancers to flourish. Although cancer researchers are trying to design better TKIs, it has so far been difficult to stay ahead of cancer cells, which can evolve very quickly, genetically rewiring themselves to thwart these drugs.
Using the lung cancer-on-a-chip system, Ingber’s team discovered that cancer cells in the air sac, initially resistant to first-generation TKIs, could be controlled by third-generation TKIs.
But the third-generation TKIs were only successful in the absence of breathing motions, as might occur when large tumors fill the lung’s alveoli and stop their motion.
“The effects of breathing motions on cancer cell behavior in our models could explain how tumor cells, which remain from a shrinking tumor after therapy, could become persister cells, able to defy drug therapy, linger and eventually cause the cancer to relapse,” said Ingber.
Altogether, the findings underscore the complexities at play in lung cancer development and the important role that true-to-human laboratory models play in improving our understanding of those mechanisms—and in the future, our ability to outsmart them therapeutically.
Other Wyss authors on the study are Christopher Chen, Girja Goyal, Alexandra Sontheimer-Phelps, Esak Lee and Oren Levy.
The study was funded by the Wyss, the Defense Advanced Research Projects Agency (DARPA cooperative agreement W911NF-12-2-0036) and the National Institutes of Health (TL1TR001410) as well as fellowships from the International Foundation for Ethical Research (IFER) and the Lymphatic Education and Research Network.