For most of their lives, our hematopoietic stem cells (HSCs)—which produce all of our blood and immune cells—are quiet and inactive. But they also are the toughest cells in the blood system, able to survive exposure to levels of radiation or viral infections that kill most other blood cells.
A new study from researchers in Columbia’s Stem Cell Initiative has discovered how HSCs cheat death, which could lead to new therapies for blood cancers and other diseases related to aging and improve stem cell transplantation.
Background
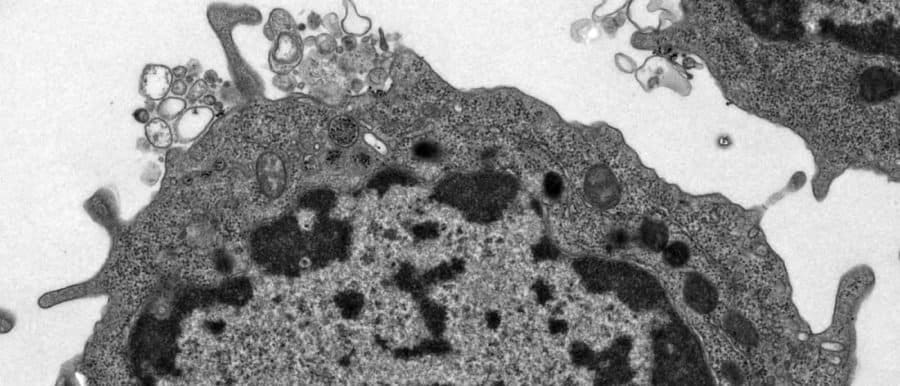
HSCs are typically quiescent and leave the work of producing new blood cells to their descendants, blood progenitor cells, which specialize in producing large quantities of specific cell types.
When infections or other inflammatory insults kill most progenitors and mature blood cells, HSCs wake up and regenerate the entire blood system.
What protects the HSCs from death and triggers them to regenerate is not well understood.
What the Researchers Found

“The finding turns the field on its head,” says Emmanuelle Passegué, PhD, director of the Columbia Stem Cell Initiative and the study’s senior author.
For years, researchers have thought TNF-alpha—a molecule released during infection and inflammation—was a danger to HSCs.
But these studies were often unable to fully separate HSCs from other types of cells. Using new and improved techniques, Passegué and postdoctoral fellow Masayuki Yamashita, PhD, found that TNF-alpha protects HSCs while triggering the death of progenitors.
HSCs survive because TNF-alpha activates a unique mechanism in HSCs that shields them from a particular form of cell death called necroptosis. Stem cells also become primed to regenerate the blood system when TNF-alpha disappears.
Survival Mechanisms Hijacked by Malignant or Aged Cells
The programs triggered by TNF-alpha may be a defense against viral infections. “Viruses can easily infect progenitor cells and turn them into virus factories,” Passegué says. “Purging these cells while preserving the stem cells can eliminate the infection and let the organism rebuild.”
But that’s only a great strategy when none of the cells are behaving badly.
The survival program that protects HSCs can be hijacked by malignant blood cells, as Passegué and Yamashita found in cells from patients with acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS).
Aged HSCs that may have acquired deleterious mutations over time can also tap the survival program to prevent death, which may lead to other age-related diseases.
“The big question now is what we can do about this,” Passegué says. “Can we kill malignant and transformed stem cells to prevent disease from progressing?”
Next Steps
By looking at the activity of a handful of genes, Yamashita and Passegué can determine if a cell will live or die in response to TNF-alpha.
That may help determine if patients with myelodysplastic syndromes—where TNF-alpha is elevated—will develop leukemia. Patients with MDS can progress rapidly to leukemia or remain stable for decades, but physicians currently have no way to make a prognosis.
Their findings also may lead to improvements in bone marrow and stem cell transplantation. Passegué and Yamashita identified a short window of time when HSCs are vulnerable to TNF-alpha exposure and necroptosis killing. This effect dramatically impairs transplantation and regeneration of the blood system; understanding the process may allow physicians to mitigate that effect.
Finally, the results also may explain rare cases of anemia and other blood disorders that have been reported with the clinical use of TNF-α inhibitors for the treatment of rheumatoid arthritis and other inflammatory diseases.