Malaria parasites are rapidly developing resistance to front-line drugs across the world, threatening to undo years of progress in reducing deaths from the disease.
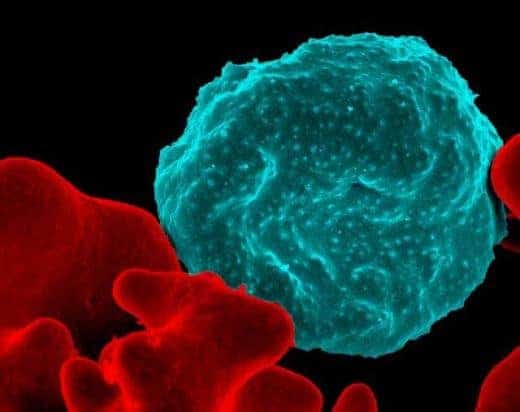
New pictures of a key mediator of drug resistance for the parasite—captured with single-particle cryo-electron microscopy by a team of scientists at Columbia University Vagelos College of Physicians and Surgeon—are now giving researchers clues about how to combat resistance.
The study, published Nov. 27 in the journal Nature, shows that drug resistance in the malaria parasite is linked to a specific protein and illustrates how mutations in the protein allow the parasite to expel the drug. The new discovery may help scientists find ways to restore the drugs’ potency and will allow health officials in other parts of the world to monitor for emerging resistance.
“The fight against malaria is stalling,” says David Fidock, PhD, the C.S. Hamish Young Professor of Microbiology & Immunology, who led the effort with Filippo Mancia, PhD, associate professor of physiology & cellular biophysics, and Matthias Quick, PhD, associate professor of neurobiology (in psychiatry). “Uncovering the molecular underpinnings of resistance is essential to prolonging the effectiveness of current drugs and developing new ones.”
Here are six take-aways from the paper:
Image shows how a frontline malaria drug is losing effectiveness
For nearly 15 years, the drug piperaquine, or PPQ, has been used all over the world to treat people infected with the malaria parasite. The drug, in combination with artemisinin, has helped slash the number of deaths caused by the disease from over 1 million in 2004 to an estimated 435,000 in 2017. The disease strikes more than 220 million individuals each year across the globe, including Africa, Southeast Asia, the Western Pacific, and South America. Almost all fatal infections occur in young African children.
But resistance to PPQ has exploded recently in Southeast Asia. “In some areas, the frontline combination of PPQ with dihydroartemisinin (which also has succumbed to resistance) is now effective in only 13% of patients, making this an essentially useless drug in those regions,” Fidock says.
This study in Nature shows that the source of PPQ resistance is a protein in the malaria parasite called PfCRT.
PfCRT is the same protein that had mediated resistance to the former first-line drug, chloroquine (CQ).
That coincidence may create new opportunities for treatment, since the new mutations, which are spreading like wildfire across Southeast Asia, often cause parasites to lose their chloroquine resistance. Combining antimalarials could treat drug-resistant and sensitive parasite infections.
Resistant parasites spit out drug
The antimalarial drugs CQ and PPQ work by entering the parasite’s digestive vacuole (a compartment resembling a stomach) and altering it so that the parasite poisons itself on its own toxic waste product, formed from digested hemoglobin.
PfCRT is located in the vacuole’s membrane, and the location of mutations—inside a central cavity of PfCRT—reaffirm the observation that resistant parasites use variant forms of this protein to expel the drug out of the vacuole.
“It looked like the protein spits the drug out of the parasite’s stomach,” says Mancia, “keeping it away from its target.”
Though the images were evocative, biochemical testing of the PfCRT’s transport properties was needed to confirm the researchers’ suspicions. By making other mutations in the protein and testing their drug binding and transport abilities, Quick found that only mutations in the protein’s central cavity give PfCRT the ability to expel the drug from the vacuole.
Scientists can now predict how resistance will arise in other parts of the world
With images of PfCRT in hand—combined with the location and properties of resistance-causing mutations—it is now possible to predict how PPQ resistance will arise in other parts of the world.
“The PfCRT gene is difficult to sequence, so it’s been hard for people to monitor,” Fidock says. “There are hundreds of locations in PfCRT that could be mutated, but now we can say just look at these handful in the central cavity with specific structural and conservation properties. They are the only ones that can drive resistance.”
Based on what’s now known, Fidock says South America could be the next place where PPQ fails. Results presented in this report already show one such mutation in PfCRT that, should it appear and spread in South America, would lead to high-grade resistance and augment the risk of treatment failures.
“Getting ahead of the ‘drug resistance curve’ by knowing where to look in the parasite’s genome will be critical to identifying where resistance arises and having time to move to alternative treatment strategies,” Fidock says.
Fidock and Quick are now testing whether PfCRT mutations identified in Asian malaria parasites will also cause PPQ resistance in African parasites, which are genetically distinct and which cause the vast majority of the global malaria burden. Those experiments may also help officials in Africa who are planning to deploy PPQ more broadly in areas of high transmission and who need to know how to monitor for signs of emerging resistance.
Study suggests ways to restore the potency of antimalarial drugs
Parasites have enlisted PfCRT in their fight against antimalarials, but researchers could also co-opt PfCRT to restore the potency of PPQ and similar drugs.
“We may be able to restore the efficacy of these drugs with an agent that entirely blocks the capacity of this protein to transport anything,” says Fidock, who is working with colleagues to develop parasite-based screens to identify potential candidate compounds.
“That would make PPQ and the earlier first-line drug chloroquine fully functional.”
Limits of Nobel technique pushed to acquire images

The malarial protein (49 kDa) is one of the smallest molecules of its type to be visualized with cryo-electron microscopy (cryo-EM), which is typically limited to proteins of at least 100 kDa in size. PfCRT needed to be bulked up with an antibody fragment before it could be seen under the electron microscope. This fragment, which was found to bind to the PfCRT central cavity, allowed the researchers to see PfCRT from multiple angles, which was necessary to generate a 3D model.
PfCRT’s small stature wasn’t the only problem in obtaining clear images by cryo-EM. PfCRT is normally surrounded by lipids inserted in a biological membrane, so the protein required the use of detergents to be extracted and purified, creating an often destabilizing and non-natural environment to image the protein. The researchers sidestepped this problem by creating nanosized lipid discs to hold PfCRT in a nearly natural state without obscuring important details from view.
The study took efforts of three labs at Columbia University
The discoveries in the new study were made possible only with the close collaboration of three laboratories at Columbia University’s Vagelos College of Physicians and Surgeons.
David Fidock’s malaria research lab had uncovered the first evidence for PfCRT’s role in resistance and mutations present in the field. This work began with a seminal report in 2000 in Molecular Cell where he and others first reported PfCRT as the cause of chloroquine resistance in the human malaria parasite Plasmodium falciparum. Drs. Fidock and Mancia started collaborating in 2013 on this project, both interested in shedding a mechanistic light on the process of resistance, but the yields of purified protein were too low for other structural biology techniques, and cryo-EM was not yet within reach to study such a small protein.
In Filippo Mancia’s structural biology lab, Jonathan Kim devised methods to obtain enough protein for the experiments and to prepare pure and homogeneous proteins suitable for imaging, a process that took several years of testing and optimization. Yong Zi Tan contributed his expertise in cryo-EM to solve PfCRT’s structure, utilizing know-how and facilities at the Simons Electron Microscopy Center at the New York Structural Biology Center.
The final confirmation of PfCRT’s role in resistance came from the lab of Matthias Quick, an expert in membrane transport processes, which measured how mutations in PfCRT affected drug binding and transport.
“This study is a first step, but it shows that we have the basic science tools at Columbia to answer important questions about malaria parasites and the spread of drug resistance in the field,” Mancia says.
“Our labs are thousands of miles from the middle of Cambodia where these changes are happening,” adds Fidock, “but our work joins the two directly together. We can now rapidly translate clinical findings about emerging resistance into detailed structural and functional understandings of how resistance works and feed that back to field workers to adjust their treatment strategies. Ultimately, these approaches are vital to ensure that we don’t let resistance gain the upper hand and that we continue to drive down the burden of this devastating infectious disease.”
Topics
References
More Information
The research was published in Nature in a paper titled, “Structure and Drug Resistance of the Plasmodium falciparum Transporter PfCRT.”
Additional authors: Kathryn J. Wicht (Columbia University Irving Medical Center), Satchal K. Erramilli (University of Chicago), Satish K. Dhingra (CUIMC), John Okombo (CUIMC), Jeremie Vendome (Schrödinger, Inc., New York), Laura M. Hagenah (CUIMC), Sabrina I. Giacometti (CUIMC), Audrey L. Warren (CUIMC), Kamil Nosol (University of Chicago), Paul D. Roepe (Georgetown University), Clinton S. Potter (CUIMC and Simons Electron Microscopy Center), Bridget Carragher (CUIMC and Simons Electron Microscopy Center), and Anthony A. Kossiakoff (University of Chicago).
The antibody fragments that were instrumental to determining the structure of PfCRT were produced in the lab of Anthony Kossiakoff, PhD, at the University of Chicago.
At the time the work was performed, Yong Zi Tan, PhD, was a graduate student in the labs of Filippo Mancia in the Department of Physiology and Cellular Biophysics at Columbia University Vagelos College of Physicians and Surgeons and of Bridget Carragher and Clint Potter in the Simons Electron Microscopy Center at the New York Structural Biology Center.
David Fidock, PhD, is also professor of medical sciences in the Department of Medicine at Columbia University Vagelos College of Physicians and Surgeons.
Matthias Quick, PhD, is also a member of the Center for Molecular Recognition at Columbia University Vagelos College of Physicians and Surgeons.
The work was supported by the NIH (R01AI147628 to Filippo Mancia, David Fidock, and Matthias Quick; R35GM132120; R01GM111980; R37AI50234; R01AI124678; R01GM119396; R01AI056312; R01AI111962; R01GM117372; T32HL120826; the Agency for Science, Technology and Research Singapore; the Simons Foundation (SF349247); and NYSTAR. Some of the work was performed at the Center for Membrane Protein Production and Analysis (COMPPÅ) (supported by NIH grant P41GM116799 to Wayne Hendrickson) and at the National Resource for Automated Molecular Microscopy at the Simons Electron Microscopy Center (supported by P41GM103310), both located at the New York Structural Biology Center.
The authors declare no competing interests.