An international research consortium led by UC San Francisco scientists has shown significant differences between the gut bacteria profiles of multiple sclerosis (MS) patients and healthy individuals, as well as between MS patients receiving different drug treatments. While some of these changes had been reported before, most are reported for the first time.
The group also uncovered novel mechanisms by which these bacteria may potentially influence disease development and treatment response.
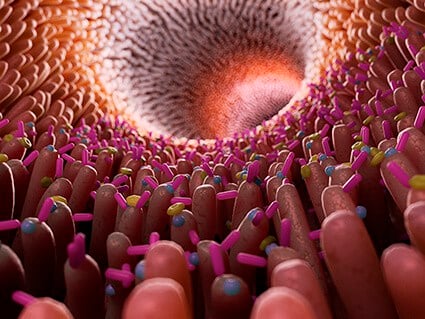
In recent years, scientists have increasingly made connections between intestinal bacteria and a number of diseases—not just diseases of the gut—including diabetes and arthritis. The field of microbiome studies really opened up with advances in DNA sequencing in the early 2010s that allowed scientists to get a detailed picture of what bacteria are present in samples of stool, blood, mucosal tissue, and skin.
Until recently, most of the experimental evidence suggesting a link between gut bacteria and MS had come from research in mice. Studies in humans had offered inconsistent results—in part because of smaller numbers of participants, and a failure to screen out the effects of the environment on an individual’s microbiome. Where one lives—rural or urban, on a mountain top or next to an oil refinery—plays a big role in the bacteria our bodies harbor.
To get around these limitations, the consortium of scientists participating in the International Multiple Sclerosis Microbiome Study (IMSMS) recruited a large number of MS patients from three continents and selected genetically unrelated controls from the same households as the patients. It was the first time this methodology had been used in such a large study. The study, which was published in Cell on September 15, 2022, describes differences between the gut microbiome profiles of 576 patients and an equal number of household controls in the United States, the United Kingdom, Spain and Argentina. The findings could lead to new therapeutics that involve either manipulating the microbiome or dietary interventions.
“This is the reference study that will be used by the field for years to come,” said Sergio Baranzini, PhD, the Heidrich Family and Friends Endowed Chair in Neurology and member of the UCSF Weill Institute for Neurosciences, who is the lead author on the new study.
With their innovative protocol, Baranzini and his colleagues were able to identify dozens of new bacteria species associated with MS and confirm other species that had previously only been associated with the disease. “We were surprised by the number of species that were differentially present in MS when compared to controls,” said Baranzini. They also found that the largest source of variation in bacteria species was linked to the geographical location of the participants, which confirmed the importance of location and local variations in diet to the gut microbiome. The second largest source of variation was a participant’s disease status, which is what the researchers had expected.
The study was the second in a series being conducted by iMSMS, an international consortium established in 2015 for the purpose of determining the role of gut bacteria in MS disease susceptibility, progression, and response to therapy. The first study validated the household control protocol, showing that it increases statistical power in population-based microbiome studies.
The findings of the study are primarily descriptive, acknowledges Baranzini. “When looking at the microbiome, there are two questions that usually are asked,” he said. “The first one is ‘Who’s there?’ This is what we’re trying to answer in this paper. The second is, ‘What are they doing?’”
Answering the second question requires mechanistic studies with individual bacteria to understand their metabolic profiles. Still, the researchers got some hints at what the bacteria they found are doing by studying the potential pathways that these bacteria encode.
“Knowing which genes from which species we are able to identify in cases and controls, we can now start to reconstruct which potential pathways are active in patients and controls,” said Baranzini.
For example, some of the bacteria the team found to be associated with MS seem to play a role in helping humans process fiber from plants, the byproducts of which tend to be found in increased concentrations in MS patients. Other species seem to have an influence on inflammation and the energy production machinery of the cell.
The researchers also found that patients treated with an immunomodulator known as interferon beta-1a, the oldest therapy for MS, have lower concentrations of short-chain fatty acids in their feces and higher concentrations in their blood. Short-chain fatty acids are known for their anti-inflammatory properties, so this suggests that interferon works by increasing the transportation of these molecules from the gut to the blood stream, which Baranzini said could be one of the mechanisms of action of interferon.
The iMSMS group will continue to recruit patients, expanding to Germany and Canada, until the total number of participants in the cohort reaches 2000. Starting this fall, they will also follow a subset of patients over two years to see how their gut microbiota change in response to treatment, lifestyle changes and disease progression. All of the data from these studies will be publicly available.
“This is an example of how big science can only be achieved collaboratively,” he added. “In the iMSMS, we really brought together the best and the brightest researchers in the microbiome research field and in multiple sclerosis, and they’re all pulling towards the same objective.”