A pilot study conducted by researchers at the Università Cattolica del Sacro Cuore in Rome, Italy, suggests that personalized “cocktails” of antibiotics, probiotics, and prebiotics may be highly effective in treating post-infection irritable bowel syndrome (PI-IBS). The findings, presented at the ESCMID Global Congress in Barcelona, Spain, offer hope for individuals suffering from this common form of IBS.
PI-IBS: A Challenging Condition
PI-IBS is a form of irritable bowel syndrome that occurs after gastroenteritis or food poisoning, with symptoms such as diarrhea, constipation, bloating, and abdominal pain persisting for months or even years after the initial infection. According to lead researcher Professor Maurizio Sanguinetti, approximately 10-30% of individuals who experience acute gastroenteritis develop PI-IBS.
“Treatment focuses on managing symptoms and improving quality of life,” says Professor Sanguinetti. “It typically involves a combination of dietary modifications, lifestyle changes, anti-diarrhoeal drugs, probiotics and other medications and psychological therapies, such as cognitive behavioural therapy.”
However, symptoms can vary widely among individuals and may not always respond to conventional therapies, making PI-IBS challenging to treat.
Personalized Gut Microbiota Therapy
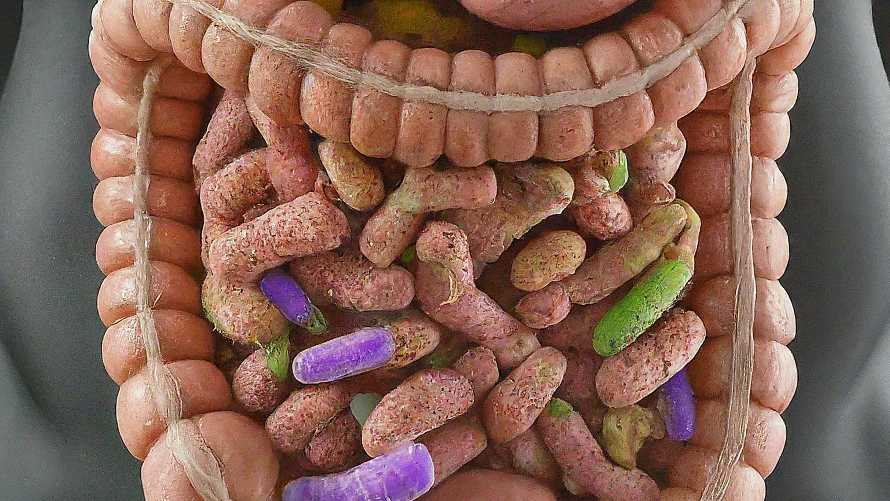
In the pilot study, 13 PI-IBS patients underwent targeted gut-microbiota therapy based on the analysis of their gut microbiota. Genetic profiling was used to identify the bacteria present in fecal samples and measure their abundance. The results revealed imbalances in the patients’ gut microbiota, such as lower than expected bacterial diversity, high levels of pro-inflammatory bacteria, and low levels of protective bacteria.
Based on these findings, personalized therapies were designed for each patient, consisting of short courses of antibiotics to reduce levels of potentially harmful bacteria, followed by prebiotics and/or postbiotics to enhance the numbers of protective bacteria and compete with the harmful bacteria for space and resources.
Twelve weeks after the start of treatment, 93% of patients experienced an improvement in symptoms, and 38.5% achieved total remission.
“A precision medicine approach, in which testing and careful analysis of the gut microbiota allows the development of personalised treatments holds great promise in the treatment of post-infection IBS,” says Professor Sanguinetti. “While rigorous larger-scale studies are needed to confirm these preliminary findings, this type of testing will likely soon be widely used in the treatment of post-infection IBS and other similar conditions.”
Keyword phrase: Personalized gut microbiota therapy for post-infection IBS