An optical imaging technique that measures metabolic activity in cancer cells can accurately differentiate breast cancer subtypes, and it can detect responses to treatment as early as two days after therapy administration, according to a study published in Cancer Research, a journal of the American Association for Cancer Research.
“The process of targeted drug development requires assays that measure drug target engagement and predict the response (or lack thereof) to treatment,” said Alex Walsh, a graduate student in the Department of Biomedical Engineering at Vanderbilt University in Nashville, Tenn. “We have shown that optical metabolic imaging (OMI) enables fast, sensitive, and accurate measurement of drug action. Importantly, OMI measurements can be made repeatedly over time in a live animal, which significantly reduces the cost of these preclinical studies.”
Human cells undergo extensive chemical reactions called metabolic activity to produce energy, and this activity is altered in cancer cells. When cancer cells are treated with anticancer drugs, their metabolic activity changes. OMI takes advantage of the fact that two molecules involved in cellular metabolism, called nicotinamide adenine dinucleotide (NADH) and flavin adenine dinucleotide (FAD), naturally emit fluorescence when exposed to certain forms of light. In this way, OMI generates distinct signatures for cancer cells with a different metabolism and their responses to drugs.
Walsh and colleagues used a custom-built, multiphoton microscope and coupled it with a titanium-sapphire laser that causes NADH and FAD to emit fluorescence. They used specific filters to isolate the fluorescence emitted by these two molecules, and measured the ratio of the two as “redox ratio.”
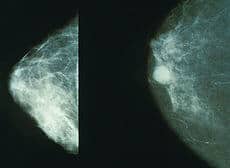
When they placed normal and cancerous breast cells under the microscope, OMI generated distinct signals for the two types of cells. OMI could also differentiate between estrogen receptor-positive, estrogen receptor-negative, HER2-positive, and HER2-negative breast cancer cells.
Next, the researchers tested the effect of the anti-HER2 antibody trastuzumab on three breast cancer cell lines that respond differently to the antibody. They found that the redox ratios were significantly reduced in drug-sensitive cells after trastuzumab treatment but unaffected in the resistant cells.
They then grew human breast tumors in mice and treated some of these with trastuzumab. When they imaged tumors in live mice, OMI showed a difference in response between trastuzumab-sensitive and -resistant tumors as early as two days after the first dose of the antibody. In comparison, FDG-PET imaging, the standard clinical metabolic imaging technique, could not measure any difference in response between trastuzumab-sensitive and -resistant tumors at any time point in the experiment, which lasted 12 days.
“Cancer drugs have profound effects on cellular energy production, and this can be harnessed by OMI to identify responding cells from nonresponding cells,” said Walsh. “We are hoping to develop a high-throughput screening method to predict the optimal drug treatment for a particular patient.”
Importantly, OMI can be used on tissues freshly excised from patients but, with further development, it could be incorporated in endoscopes for live imaging of human cancers, according to the investigators.
This study was funded by the National Institutes of Health, the National Science Foundation, the Department of Defense Breast Cancer Research Program, Vanderbilt-Ingram Cancer Center, and Vanderbilt University Medical Center. The authors have no conflicts of interest to disclose.

Hello!
I’ve started the petition “President Barack Obama: Fund research on the mouse mammary tumor virus.” and need your help to get it off the ground.
Will you take 30 seconds to sign it right now? Here’s the link:
http://www.change.org/petitions/president-barack-obama-fund-research-on-the-mouse-mammary-tumor-virus
Here’s why it’s important:
A significant proportion of human breast cancers – 40 percent – contain gene sequences that are very similar to that of a retrovirus that is known to cause breast cancer in mice. The research behind a potential human mammary tumor virus is marching forward steadily, as Drs. Pogo, Etkind, and Melena study the statistical analysis and biochemical pathways of the potential virus.
A virus works by first replicating in a primary cell and infecting supplementary cells as it grows and divides. Human breast cells divide with the circulating estrogen hormone. When the breast cell with the viral gene sequence divides, it releases viral particles that poison other breast cells and causes a cycle of infection.
If we can determine that the mouse mammary tumor virus causes as much as 40 percent of breast cancers, we could focus on creating a vaccine to prevent the disease in women. This could lead to a significant gain for The Pure Cure: the primary prevention of breast cancer.
However, we need further funding to determine whether this virus could potentially cause breast cancer in women. We implore President Obama and his administration to focus their research spending toward the mouse mammary tumor virus. If we can find the causes of breast cancer and potentially create a vaccine to prevent breast cancer, we could save the lives of hundreds of thousands of women around the country.
Over the last five years, Dr. Kathleen T. Ruddy, breast cancer surgeon and Founder of the Breast Health and Healing Foundation, has focused all her efforts onto moving forward with this research and preventing the disease. The documentary filmmaker Steve Zukerman is currently developing a film about Dr. Ruddy’s efforts and the researchers working on the possibility that a virus may cause breast cancer. The movement toward primary prevention is marching forward. Will you join our cause?
Thanks!
Vera Viner