For the worst cases of type 1 diabetes, islet transplantation already has freed hundreds of people from complete dependence on insulin and from life-threatening consequences of the disease.
However, the procedure still is regarded as experimental by the U.S. Food and Drug Administration (FDA).
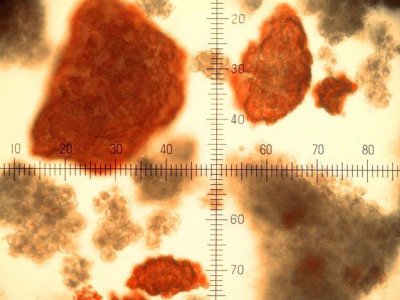
Islets are clusters of insulin-making cells in the pancreas that are destroyed in people with type 1 diabetes. After transplanting islet cells from a donor pancreas, the new islet cells can begin to produce insulin.
“Overall the results of islet transplantation are much better than they used to be,” said UC San Francisco transplant surgeon Andrew M. Posselt, MD, PhD, “We’re approaching results as good as we see with whole pancreas transplants.”
Posselt, who co-directs the Clinical Islet Transplant Program at UCSF, is part of an international push to bring islet transplantation into the mainstream. As part of that movement, experts gathered in Monterey in September for 14th World Congress of the International Pancreas and Islet Transplant Association (IPITA). World Congress chair, Peter Stock, MD, PhD, is the other co-lead of the UCSF program.
The meeting – sponsored by IPITA, the Transplantation Society and the Department of Surgery at UCSF – included discussions on new ways to foster long-term survival of transplanted islets and to prevent their rejection by the immune system, which is the key to controlling blood sugar without reliance on precisely administered insulin injections.
From Whole Pancreas to Islets
Whole-organ pancreas transplantation has for many years been an option in cases of type 1 diabetes or in cases in which kidney failure – a complication of the disease – makes it more practical for surgeons to transplant a kidney and pancreas at the same time.
Pancreas transplantation is an invasive surgery, unsuited for many elderly patients or for those with cardiovascular disease. Islet transplantation does not require major surgery and involves much less tissue.
In fact, islets make up less than 2 percent of the volume of the pancreas. They are the only pancreatic tissue destroyed by type 1 diabetes, a disease caused by an autoimmune response in which the immune system attacks specific molecules on islets. The rest of the pancreas continues to play its normal role in aiding the digestion of food.
For transplantation, islets are extracted from a donated pancreas, purified from surrounding cells and tissue and infused into the portal vein, where they lodge in the smallest blood vessels and begin to secrete insulin in response to blood glucose levels.
After a successful transplant, the patient gains better control over glucose levels in the blood and may no longer require insulin injections. This is because transplanted islets not only secrete insulin, but also because – like a healthy pancreas – the transplanted islets know how much insulin to secrete and also secrete other hormones important for glucose control.
In comparison to what islets cells can deliver, insulin injections are a crude means of controlling glucose levels.
“After you have had a successful islet transplant, even if you are taking a bit of insulin, the multiple regulatory hormones secreted by the islets completely prevent low blood sugars,” Posselt says. “That’s what is really liberating to the patients: They don’t need to worry about waking up at night to check their sugars, or about driving or doing other daily activities and suddenly developing a dangerously low blood glucose.”
Momentum for Islet Transplantation
Early experiments in islet transplantation were considered failures, but interest has been rekindled since 2000, when researchers from the University of Alberta in Edmonton developed a new islet-transplant protocol that increased insulin-independence rates from about 15 percent to about 80 percent, Posselt said.
The Edmonton protocol eliminated glucocorticoid steroid drugs – which can harm islets – as an immunosuppressive agent, and relied instead on other immunosuppressants. For each patient, the Edmonton researchers obtained islets from several organ donors to make sure they all received adequate amounts. Within a few years, many study participants again became dependent on insulin, but researchers saw the potential to save lives.
Today, procedures for obtaining islets and immunosuppressive protocols continue to be refined at experimental centers sanctioned by the FDA. UCSF, having launched a state-of-the-art islet preparation facility, participates with several other major medical centers in the Clinical Islet Transplantation (CIT) Consortium to evaluate protocols developed by the National Institutes of Health.
“We have spent a lot of time training people at other sites,” Posselt said. “We are trying to standardize protocols for islet isolation and transplantation to reliably obtain successful results across hospitals for patients with life-threatening diabetes. We want to demonstrate the value of the treatment to insurers and maximize the number of patients who can benefit.”
Donor tissue is always in short supply. A key to better islet transplantation is to use only one donor’s pancreas to obtain enough islets.
In addition to choosing appropriate donors, a key to accomplishing this is to prevent the harvested islet cells from dying.
“As the efficacy of isolating islets improves, our ability to make patients insulin-independent after receiving islets from a single donor is becoming much better,” Posselt said. “Furthermore, if a patient can achieve independence after a single donor transplant, the cost is actually lower than for a whole pancreas transplant.”
An islet transplantation costs about $20,000 dollars, according to a study of UCSF transplants presented at the World Congress by Posselt and colleagues.
UCSF researchers also are pioneering new transplant procedures, including new drug treatments to battle islet destruction. The immune system’s normal rejection response to foreign islets remains a challenge to the survival of transplanted cells, and so does the original autoimmune response that first triggered the immune system to attack and destroy the patient’s own islets.
T Cells: Good Cops, Bad Cops
UCSF scientists have for years explored strategies for blunting the autoimmune response in type 1 diabetes, blamed largely on a subclass of the immune system’s T cells known as effectors.
In clinical trials aimed at halting the advance of islet destruction, they are using drugs that knock down these effector T cells. Similarly targeted drugs have been incorporated into islet transplant protocols.
However, there is a “good cop” to counter the effector T cell’s “bad cop” role in type 1 diabetes. The good cops, rare cells called T regulatory cells, or TREGs, can dampen autoimmune responses.
Pioneering TREG researchers at UCSF – Jeffrey Bluestone, PhD, the A.W. and Mary Margaret Clausen Distinguished Professor of Metabolism and Endocrinology and Qizhi Tang, PhD, director of the Transplantation Research Laboratory at UCSF – have been developing ways to boost TREG populations in the hopes of coaxing the immune system to tolerate its own tissue in autoimmune diseases such as type 1 diabetes, and to accept foreign tissue during transplantation.
One approach is to take some of a patient’s TREGs and to stimulate their proliferation in lab-grown cultures before returning them to the patient.
In addition, Tang, working with Posselt and colleagues, found that some new drug treatments can also boost the proportion of TREGs in the blood. In a study presented at the World Congress, the researchers compared an islet transplant protocol that included treatment with efalizumab – an anti-inflammatory psoriasis and rheumatoid arthritis drug – to a more commonly used alternative.
Efalizumab not only better suppressed effector T cells, but also dramatically increased TREG populations in the five patients who received it. One patient who had very high TREG levels had to be taken off all immunosuppression due to complications resulting from activation of latent Epstein-Barr virus. She recovered, and so far has remained insulin-independent without any immunosuppression for one year.
The result raises hope that lifelong immunosuppression one day may no longer be routinely required following islet transplantation.
Tang likens immunosuppressant dosing to Goldilocks’ effort to find the porridge or bed that is just right: With too much immunosuppression, infections or malignancies become life-threatening, but with too little, transplant rejection occurs.
Looking Beyond Human Donors
Even if researchers get everything “just right” with islet transplant protocols, donor shortages will remain a problem, Tang says.
To address the shortage, scientists are exploring alternatives, such pig islet cells, or new islets developed from human stem cells. These options pose their own unique challenges, Tang said.
Matthias Hebrok, PhD, director of the UCSF Diabetes Center, has been working to develop islet cells from embryonic stem cells – immortal cells that might be used to develop a limitless supply of islets.
Recent advances with stem cells grown in the lab offer encouraging signs that functioning, insulin-secreting islets can be generated outside the body, according to Hebrok.
Similarly, Bluestone is working with San Diego-based ViaCyte Inc. to design and launch clinical trials of pro-islet cells developed from embryonic stem cells. These cells are expected to mature and secrete insulin in a naturally regulated manner within the body.
Embryonic stem cells once were viewed as the ultimate source of transplant tissue that would not cause rejection, but unfortunately that’s not the case, Tang said.
“For a while, people believed that stem cells were not immunogenic – that they were invisible to the immune system,” she said. “Our work now shows that the immune cells can see them and completely destroy them as they would any graft.”
Pig islets pose their own complicated problems, Tang said. Being from a different species, pig islets are too immunogenic. The amount of immunosuppression required to stop rejection would cripple the immune system in fighting infection, according to Tang.
As a solution, Tang said, several researchers, including scientists at ViaCyte and Tejal Desai, PhD, and Shuvo Roy, PhD, both professors of bioengineering and therapeutic sciences at UCSF, have been working on ways to encapsulate transplanted stem-cell-derived or pig islet cells, a strategy that would shield against attacks by the immune system.
“I still view immunological issues as the main ones to overcome in islet transplantation,” Tang said. “If we can overcome them, it will open up the field, and we will be able to help many more patients.”


See new book:
Transplant Handbook for Patients:
Replacing Stem Cells in Your Bone Marrow.
http://TransplantHandbook.com
–Dan Poynter, Day +110 since transplant.