Fragmented REM sleep may hinder effective treatment of mental health condition
The effectiveness of post-traumatic stress disorder (PTSD) treatment may hinge significantly upon sleep quality, report researchers at the University of California, San Diego School of Medicine and Veterans Affairs San Diego Healthcare System in a paper published today in the Journal of Neuroscience.
“I think these findings help us understand why sleep disturbances and nightmares are such important symptoms in PTSD,” said Sean P.A. Drummond, PhD, professor of psychiatry and director of the Behavioral Sleep Medicine Program at the VA San Diego Healthcare System. “Our study suggests the physiological mechanism whereby sleep difficulties can help maintain PTSD. It also strongly implies a mechanism by which poor sleep may impair the ability of an individual to fully benefit from exposure-based PTSD treatments, which are the gold standard of interventions.
“The implication is that we should try treating sleep before treating the daytime symptoms of PTSD and see if those who are sleeping better when they start exposure therapy derive more benefit.”
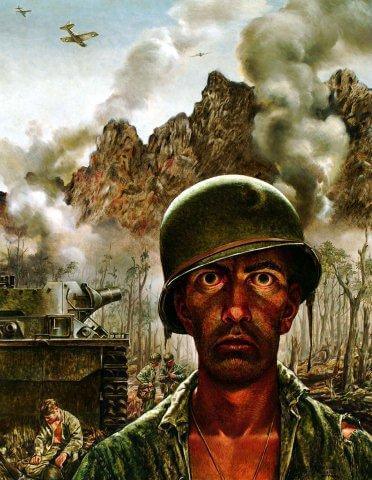
PTSD is an often difficult-to-treat mental health condition triggered by a terrifying event. It is frequently associated with persons who have served in war zones and is characterized by severe anxiety, flashbacks, nightmares and uncontrollable thoughts, often fearful. Research has shown that fear conditioning, considered an animal model of PTSD, results in disruption of animals’ rapid eye movement (REM) sleep – periods of deeper, dream-filled slumber. Fear conditioning is a form of learning in which the animal model is trained to associate an aversive stimulus, such as an electrical shock, with a neutral stimulus, such as a tone or beep.
Drummond and colleagues investigated the impact of fear conditioning – and another form of behavioral training called safety signal learning – upon human REM sleep, using 42 healthy volunteers tested over three consecutive days and nights. Safety signals are learned cues that predict the non-occurrence of an aversive event.
“We examined the relationship between REM sleep and the ability to learn – and consolidate memory for – stimuli that represent threats and that represent safety,” said Drummond.
“In PTSD, humans learn to associate threat with a stimulus that used to be neutral or even pleasant. Often, this fear generalizes so that they have a hard time learning that other stimuli are safe. For example, a U.S. Marine in Iraq might suffer trauma when her personnel carrier is blown up by road side bomb hidden in trash alongside the road. When she comes home, she should learn that trash on the side of I-5 does not pose a threat – it’s a safe stimulus – but that may be difficult for her.”
The researchers found that increased safety signaling was associated with increased REM sleep consolidation at night and that the quality of overnight REM sleep was related to how well volunteers managed fear conditioning.
Drummond said stimuli representing safety increased human REM sleep and that “helps humans distinguish threatening stimuli from safe stimuli the next day. So while animal studies focused on learning and unlearning a threat, our study showed REM sleep in humans is more related to learning and remembering safety.”
He noted, however, that the findings are not conclusive. No comparable animal studies, for example, have examined the relationship between safety and REM sleep. Nonetheless, the findings do encourage further investigation, eventually into human PTSD populations where fear, safety and sleep are on-going and paramount concerns among military veterans and others.
“A very large percentage of missions in both Iraq and Afghanistan were at night,” said Drummond, who is also associate director of the Mood Disorders Psychotherapy Program at VA San Diego Healthcare System. “So soldiers learned the night was a time of danger. When they come home, they have a hard time learning night here is a time to relax and go to sleep.”
Co-authors include Anisa J. Marshall, VA San Diego Healthcare System; Dean T. Acheson and Victoria B. Risbrough, VA San Diego Healthcare System and Department of Psychiatry, UCSD; and Laura D. Straus, VA San Diego Healthcare System and SDSU-UCSD Joint Doctoral Program in Clinical Psychology.
Funding support came, in part, from the Defense Medical Research and Development Program (DM102425). Infrastructure support provided by VA San Diego Center for Excellence in Stress and Mental Health.