Doctors treating patients battling both HIV and tuberculosis (TB)—many of whom live in Africa—are faced with the decision when to start those patients on antiretroviral therapy (ART) while they are being treated with antibiotics for active TB disease. Some patients fare well on both interventions, with the immune system in check and the TB controlled. Others undergo complications from TB, such as paradoxical immune reconstitution inflammatory syndrome (IRIS), a worsening of TB symptoms despite response to therapy, while still others experience immune failure and early death. The best way to determine which patients go on to develop IRIS or die after treatment begins is not fully understood.
Now, reporting in a new study published online this week in The Lancet Infectious Diseases, researchers under the Botswana-UPenn Partnership at the University of Pennsylvania, including Shruthi Ravimohan, PhD, a research associate in the division of Infectious Diseases at Penn’s Perelman School of Medicine, and Gregory P. Bisson, MD, MSCE, an assistant professor in the division of Infectious Diseases and a senior scholar at the Center for Clinical Epidemiology and Biostatistics, have identified immune biomarkers in patients before they begin ART that could help distinguish these two groups.
“The different immune and inflammatory responses in these patients can tell us something very valuable that helps inform future treatment strategies,” Ravimohan said. “Most importantly, our findings show that advanced HIV/TB patients are a heterogeneous population that should not be treated uniformly with response to immune interventions.”
Past studies have focused on outcomes for TB-IRIS, but none have compared immune responses and biomarker profiles among patients who died early versus those who experienced IRIS.
The findings are of particular importance to health care providers in places where co-infections are common and resources are limited, such as Africa. Potentially, some of the biomarkers could be measured with a simple, currently available blood test that could help guide physicians on treatment strategies.
There are estimated to be over one million people worldwide who have TB and HIV co-infection, though the burden of disease through HIV/TB is particularly high in sub-Saharan Africa; it’s also becoming a growing concern in Asia. A recent study showed that up to 20 percent of patients died within 48 weeks, despite starting both ART and TB medications.
The prospective study of 201 patients in Botswana, who were evaluated pre and post ART, revealed that lower levels of eight biomarkers, including IL-6, IL-15 and GM-CSF, pre-ART were independently associated with an increased risk of IRIS, while higher levels of MCP-1 and TNF-alpha were independently associated with an increased risk of death. However, IRIS and early mortality patients both experienced rapid increases in immune activation and inflammation after initiating ART. Four biomarkers, including IL-6, TNF-alpha, and G-CSF, were independently associated with an increased risk of TB-IRIS, and five biomarkers were associated with an increased risk of death, including IL-1RA and G-CSF.
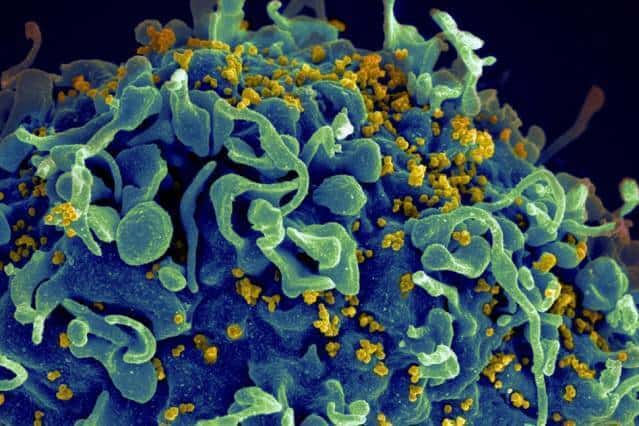
The magnitude of early immune recovery (CD4 cell count) differed drastically between the two after being in ART, as well, underscoring the need for a personalized approach in these two groups. Those who initiated ART and died early had an increase in inflammation without the immune system rebounding enough to control the TB, while IRIS patients recovered more quickly.
Click here to view the full release.