Tracking changes in the eye’s retina may help doctors provide more effective treatment for people with schizophrenia, according to researchers at Rutgers University and Mount Sinai’s New York Eye and Ear Infirmary.
A link between vision problems and schizophrenia is well established, with as many as 62 percent of adult patients with schizophrenia experiencing visual distortions involving form, motion or color. Researchers reported on and summarized multiple, replicated indicators of eye abnormalities in schizophrenia in a literature review published online in the journal Schizophrenia Research: Cognition.
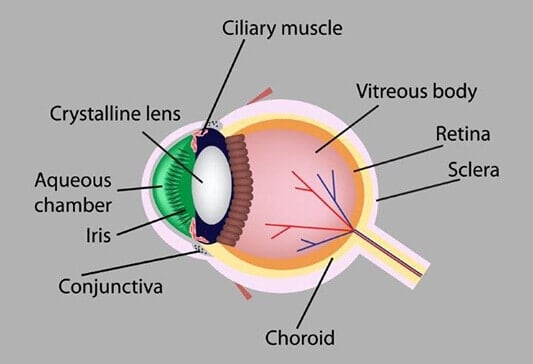
They described a widening of small blood vessels in the eyes of schizophrenia patients, and in young people at high risk for the disorder, perhaps caused by chronic low oxygen supply to the brain – which they said could explain vision changes and signal disease risk and progression. They also found a thinning of the retinal nerve fiber layer, known to be related to the onset of hallucinations and visual acuity problems in patients with Parkinson’s disease.
“Our analysis of many studies suggests that measuring retinal changes may help doctors in the future to adjust schizophrenia treatment for each patient,” said study co-author Richard B. Rosen, director of ophthalmology research, New York Eye and Ear Infirmary of Mount Sinai, and an ophthalmology professor at the Icahn School of Medicine at Mount Sinai. “More studies are needed to drive the understanding of the contribution of retinal and other ocular pathology to disturbances seen in these patients, and our results will help guide future research.”
Abnormalities in the way the brain processes visual information contribute to the difficulties people with schizophrenia have with social interactions and in recognizing what is real. That makes it harder for them to track moving objects, perceive depth, draw contrast between light and dark or different colors, organize visual elements into shapes and recognize facial expressions, according to previous research. One past study also found that poorer visual acuity at age 4 predicted a diagnosis of schizophrenia in adulthood, and another that children who later develop schizophrenia have elevated rates of strabismus, or misalignment of the eyes, compared to the general population.
Rosen and co-author Steven M. Silverstein, director of the division of schizophrenia research at Rutgers University Behavioral Health Care and Robert Wood Johnson Medical School Department of Psychiatry, examined the results of approximately 170 existing studies. They grouped the findings into multiple categories, including changes in the retina compared with those in other parts of the eye, and changes related to dopamine compared with those related to other neurotransmitters, key brain chemicals associated with the disease.
Interestingly, the analysis uncovered no reports of people with schizophrenia who were born blind, suggesting that congenital blindness may completely or partially protect against the development of schizophrenia. Because congenitally blind people tend to have cognitive abilities in certain domains (such as attention) that are superior to those of sighted individuals, understanding brain re-organization after blindness may have implications for designing cognitive remediation interventions for people with schizophrenia.
“The retina develops from the same tissue as the brain,” Rosen said. “Thus retinal changes may parallel or mirror the integrity of brain structure and function. When present in children, these changes may suggest an increased risk for schizophrenia in later life. Additional research is needed to clarify these relationships, with the goals of better predicting emergence of schizophrenia, and of predicting relapse and treatment response and people diagnosed with the condition.”
In addition, the research found abnormal electrical responses by retinal cells exposed to light (as measured by electroretinography), suggesting possible cellular-level differences in the eyes of schizophrenia patients.
Vision has been understudied in schizophrenia, and studies of the retina and other ocular structures in the disorder are in their infancy, Silverstein said.
“Because it is much faster and less expensive to obtain data on retinal structure and function, compared to brain structure and function, measures of retinal and ocular structure and function may have an important role in both future research studies and the routine clinical care of people with schizophrenia,” he said.