We’re living longer. The number of U.S. adults 65 and older — roughly 40 million as of the 2010 census — is expected to nearly double to 71 million by 2030 and to reach 98 million by 2060. In much of the rest of the world, the story is the same. But if the aging trend illustrates the success of public health strategies, it also raises the specter of a major public health crisis — a sharp rise in the number of people living with Alzheimer’s disease.
Ron Brookmeyer, a professor in the UCLA Fielding School of Public Health’s Department of Biostatistics, has called attention to the looming Alzheimer’s epidemic through widely cited studies in which he has employed sophisticated computer models to project the number of cases, as well as the potential positive impact of future therapies and other strategies to prevent or delay the onset and progression of symptoms.
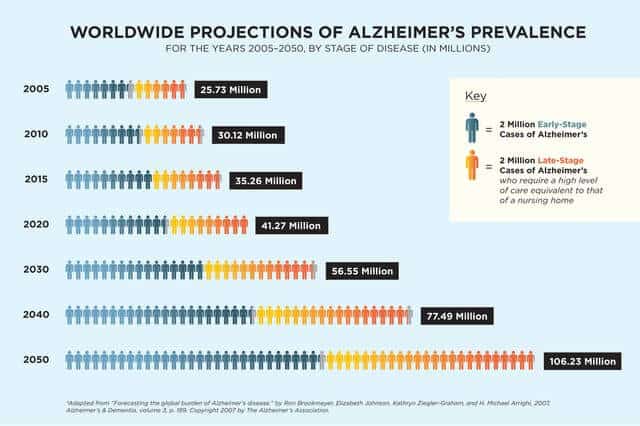
Brookmeyer’s work in this arena began nearly 20 years ago with a paper he wrote in the American Journal of Public Health projecting that the prevalence of Alzheimer’s disease in the United States would nearly quadruple by the middle of this century, by which time approximately 1 in 45 Americans will be afflicted. His 2007 study also projected that 1 in 85 persons worldwide will be living with the disease by 2050, with nearly half of them requiring a level of care equivalent to that of a nursing home.
Brookmeyer’s development of statistical models to make forecasts on epidemics began in the late 1980s with HIV/AIDS, but after becoming involved in a study on aging, he turned his attention to the threat posed by Alzheimer’s disease. “Obviously it’s not a transmissible epidemic like the ones I had been looking at, but with the aging of the population, it was clear that the numbers were going to explode,” he explains.
As part of his modeling, Brookmeyer and his colleagues consider both demographic trends and the severity of the progression of the disease. “This is a long illness,” he says. “Once you’re diagnosed, you might live with it for 10 or more years, and the intensity of the care required will vary during that time. From a public health point of view, it’s very important to look at where people will be in different stages of the disease and the needs we will be facing as a society.”
Through a systematic review of Alzheimer’s studies, Brookmeyer’s team has found that the rate of being diagnosed with the disease doubles every five years in older populations. For example, the likelihood of a diagnosis at age 77 is approximately 1 percent; by age 82 it is 2 percent, and at age 87 it is 4 percent. This rate of increase with aging is consistent across the world. Combining those factors with trends in other causes of aging-related mortality, such as cardiovascular disease and cancer, the group forecasts the future prevalence of Alzheimer’s disease.
Equally important, the modeling also allows Brookmeyer and colleagues to factor in the future impact of advances in Alzheimer’s disease prevention and treatment — what Brookmeyer calls “what if” scenarios.
“What if we could delay the onset of the disease for a few years?” he says. “In an aging population, even modest advances could be home runs in terms of their public health impact.” For example, Brookmeyer has found that if an intervention could delay the average disease onset by even a single year, it would reduce by 9 million the number of projected worldwide cases by mid-century.
Brookmeyer is currently working with researchers at UC Irvine on a study of “the oldest old” — persons over the age of 90, the fastest- growing segment of the U.S. population — to better understand the predictors of successful aging and factors that might protect against dementia. The study follows a cohort of individuals living in a retirement center who, as far back as the 1980s, began filling out detailed questionnaires designed to capture lifestyle characteristics. “Over the next 50 years in the U.S., the over-90 population is going to grow six-fold, so this is a very important group to understand when it comes to the issue of dementia,” Brookmeyer says.
While Brookmeyer’s projections of the increase in Alzheimer’s paint a bleak picture, given the current state of prevention and treatment, he points out that recent developments in the field offer plenty of room for optimism.
There have been new insights into how the disease develops, as well as the identification of new biomarkers that can assist in diagnosing Alzheimer’s and tracking the impact of potential therapies. “Among the most promising interventions currently under investigation are those that target the buildup of amyloid beta proteins in an effort to slow the onset and progression of Alzheimer’s,” Brookmeyer says.
Brookmeyer is now developing new models to better understand the potential impact of these so-called anti-amyloid beta interventions.
“The projected increase in Alzheimer’s cases represents a huge public health problem when you think about the costs associated with caring for a person with the disease, along with the emotional burden for family members. And yet funding for Alzheimer’s disease studies represents a relatively small part of the overall federal research budget,” Brookmeyer says. “With better understanding and tools we now have, the time is ripe for an investment in research that will help us address this major public health threat.”