A new study published today in the science journal Proceedings of the Royal Society B indicates that chronic exposure to an environmental toxin may increase risk of neurodegenerative illness. Conducted by scientists at the Institute for EthnoMedicine, a non-profit medical research organization, and the University of Miami Brain Endowment Bank, the study provides a foundation for future research in Alzheimer’s disease, ALS and Parkinson’s disease.
Brain tangles and amyloid deposits are the hallmarks of both Alzheimer’s disease and an unusual illness suffered by Chamorro villagers on the Pacific Island of Guam, whose diet is contaminated by the environmental toxin BMAA. Pacific Islanders with this unusual condition also suffer from dementia and symptoms similar to Alzheimer’s disease, ALS and Parkinson’s disease.
The cause of neurodegenerative disease remains largely unknown, and the role of environmental factors in these illnesses is poorly understood. However, scientists have suspected a link between BMAA, a neurotoxin found in some harmful algal blooms, and neurodegenerative illness.
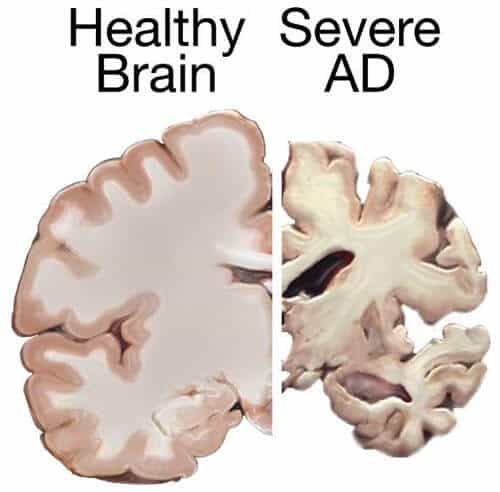
“Our findings show that chronic exposure to BMAA can trigger Alzheimer’s-like brain tangles and amyloid deposits,” said Paul Alan Cox, Ph.D., an ethnobotanist at the Institute for EthnoMedicine and lead author of the study. “As far as we are aware, this is the first time researchers have been able to successfully produce brain tangles and amyloid deposits in an animal model through exposure to an environmental toxin.”
Researchers conducted two experiments on vervets that lasted for 140 days. In the first experiment, vervets fed fruit dosed with BMAA developed neurofibrillary tangles and amyloid deposits similar to Pacific Islanders who died from the disease. Vervets fed equal amounts of L-BMAA and the dietary amino acid L-serine had a reduced density of tangles. Vervets fed a placebo dose did not develop neuropathology.
A replication experiment was conducted which added a BMAA dose closer to the amount Chamorro villagers would be exposed to over a lifetime. The first group received fruit containing L-BMAA, the second group received fruit containing one-tenth of the regular dose of L-BMAA, the third group received fruit containing equal amounts of L-BMAA and L-serine, and the fourth group received fruit containing a placebo.
“This study takes a leap forward in showing causality — that BMAA causes disease,” said Deborah Mash, Ph.D., director of the University of Miami Brain Endowment Bank and co-author of the study. “The tangles and amyloid deposits produced were nearly identical to those found in the brain tissue of the Pacific Islanders who died from the Alzheimer’s-like disease.”
After 140 days, tangles and amyloid deposits were found in the brain tissues of all of the vervets who consumed BMAA. However, there was a significant reduction in the density of tangles in those that consumed equal amounts of L-serine.
Cox does not advocate patients taking L-serine at this time. “The FDA has not approved its use for the treatment of neurodegenerative illness, and much more research is needed,” he said. “However, this new animal model may prove useful in evaluating other potential new Alzheimer’s drugs.”
The Institute has sponsored FDA-approved human clinical trials to study the effects of the naturally-occurring amino acid L-serine in people with ALS, and is working with Dartmouth Medical School to begin a Phase I human clinical trial of L-serine for patients diagnosed with mild cognitive impairment or early stage Alzheimer’s disease.