The brains of some people with autism spectrum disorder grow faster than usual early on in life, often before diagnosis. A new study co-led by Salk Institute scientists has employed a cutting-edge stem cell technique to unravel the mechanisms driving the mysterious phenomenon of excess brain growth, which affects as many as 30 percent of people with autism.
The findings, published July 6, 2016 in the journal Molecular Psychiatry, show that it is possible to use stem cell reprogramming technologies developed in the past decade to model the earliest stages of complex disorders and to evaluate potential therapeutic drugs.
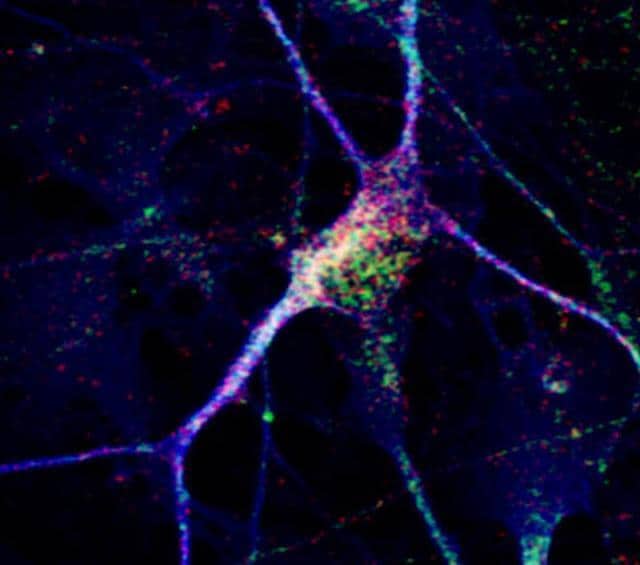
Intriguingly, the Salk team found that stem cell-derived neurons made fewer connections in the dish compared to cells from healthy individuals. Furthermore, the scientists were able to restore communication between the cells by adding IGF-1, a drug currently being evaluated in clinical trials of autism.
“This technology allows us to generate views of neuron development that have historically been intractable,” says senior investigator Rusty Gage, a professor in Salk’s Laboratory of Genetics and holder of the Vi and John Adler Chair for Research on Age-Related Neurodegenerative Diseases. “We’re excited by the possibility of using stem cell methods to unravel the biology of autism and to possibly screen for new drug treatments for this debilitating disorder.”
Autism, which affects approximately 1 out of every 68 children in the United States, is characterized by problems communicating, difficulties interacting with others, and in repetitive behaviors, although the symptoms range dramatically in type and severity. There is no known cause of autism.
In 2010, Gage, Carol Marchetto of Salk’s Laboratory of Genetics, Alysson Muotri of the University of California, San Diego, and their collaborators showed they could recreate features of Rett syndrome–a rare disorder that shares features of autism but is caused by mutations in a single gene–in a petri dish.
They did so by taking skin cells from patients, adding a mix of chemicals that instructed those cells to form stem cells, and in turn, coaxing their new stem cells into neurons. The ability to form what’s called induced pluripotent stem cells (iPSCs) from human cells was pioneered by researchers in 2007, but some scientists were initially skeptical that the new technology could lend insight into complex heritable disorders such as autism.
“In that study, induced pluripotent stem cells gave us a window into the birth of a neuron that we would not otherwise have,” says Marchetto, a senior staff scientist and the study’s first author. “Seeing features of Rett syndrome in a dish gave us the confidence to next study classical autism.”
In the new study, collaborating with Muotri and other scientists at UCSD once more, Gage’s team created stem cells from a subset of people with autism whose brains had grown up to 23 percent faster than usual during toddlerhood but had subsequently normalized.
The neuron precursor cells derived from the patients multiplied faster than those of typically developing individuals. The finding supports a theory some experts have put forth that brain enlargement is caused by disruptions to the cell’s normal cycle of division, Marchetto says. In addition, the stem cell-derived neurons of individuals with autism behaved abnormally, bursting with activity less often compared with those cells of healthy people.
Those neurons’ activity seemed to improve by adding IGF-1, which is known to enhance the connections between neurons. The group plans to use the patient cells to investigate the molecular mechanisms behind IGF-1’s effects, in particular probing for changes in gene expression with treatment.
Although the newly derived cells are far from patients’ brains, a brain cell by itself may reveal important clues about a person, Marchetto says. “It never fails to amaze me when we can see similarities between the characteristics of the cells in the dish and the human disease,” she adds.