University of Wisconsin-Madison Alzheimer’s researchers have identified a scientific approach that may help predict which older adults are more likely to develop cognitive symptoms of Alzheimer’s disease well before the onset of dementia.
This approach – which statistically analyzes a panel of biomarkers – could help identify people most likely to benefit from drugs or other interventions to slow the progress of the disease. The study was published in the August edition of the journal Brain.
“The Alzheimer’s Association estimates that if we had a prevention that merely pushed back the clinical symptoms of the disease by five years, it would almost cut in half the number of people projected to develop dementia,’’ says Annie Racine, a doctoral candidate and the study’s lead author. “That translates into millions of lives and billions of dollars saved.”
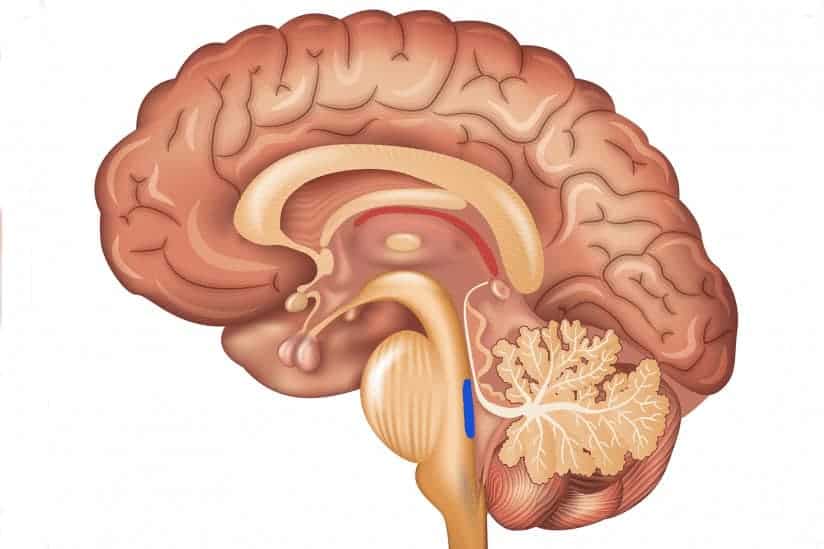
Dr. Sterling Johnson, the study’s senior author, says that while brain changes – such as the buildup of beta-amyloid plaques and tangles of another substance called tau – are markers of the disease, not everyone with these brain changes develops Alzheimer’s symptoms.
“Until now, we haven’t had a great way to use the biomarkers to predict who was going to develop clinical symptoms of the disease,’’ Johnson says. “Although the new algorithm isn’t perfect, now we can say with greater certainty who is at increased risk and more likely to decline.”
The research team recruited 175 older adults at risk for Alzheimer’s disease, and used statistical algorithms to categorize them into four clusters based on different patterns and profiles of pathology in their brains. Then, the researchers analyzed cognitive data from the participants to investigate whether these cluster groups differed on their cognitive abilities measured over as many as 10 years.
As it turns out, the biomarker panels were predictive of cognitive decline over time. One cluster in particular stood out. The group that had a biomarker profile consistent with Alzheimer’s – abnormal levels of tau and beta-amyloid in their cerebrospinal fluid – showed the steepest decline on cognitive tests of memory and language over the 10 years of testing. About two-thirds of the 22 people sorted into this group were also positive for the APOE4 gene—the greatest known risk factor for sporadic Alzheimer’s disease—compared with about one-third in the other clusters.
At the other end of the spectrum, the largest group, 76 people, were sorted into a cluster that appears to be made up of healthy aging individuals. They showed normal levels on the five biomarkers and did not decline cognitively over time.
In between, there were two clusters that weren’t classified as Alzheimer’s but who don’t seem to be aging normally either. A group of 32 people showed signs of mixed Alzheimer’s and vascular dementia. They had some of the amyloid changes in their cerebrospinal fluid, but also showed lesions in their brains’ white matter, which indicate scarring from small ischemic lesions which can be thought of as minor silent strokes.
The other cluster of 45 people had signs of brain atrophy, with brain imaging showing that the hippocampus, the brain’s memory center, was significantly smaller than the other groups. The authors speculate this group could have intrinsic brain vulnerability or could be affected by some other process that differentiates them from healthy aging. Both the in-between clusters showed non-specific decline on a test of global cognitive functioning, which further differentiates them from the healthy aging cluster.
The study participants came from a group of more than 1,800 people enrolled in two studies – the Wisconsin Alzheimer’s Disease Research Center (WADRC) study and the Wisconsin Registry for Alzheimer’s Prevention (WRAP). Both groups are enriched for people at risk for getting Alzheimer’s because about ¾ of participants have a parent with the disease.
“This study shows that just having a family history doesn’t mean you are going to get this disease,” Johnson says. “Some of the people in our studies are on a trajectory for Alzheimer’s, but more of them are aging normally, and some are on track to have a different type of brain disease.” A comprehensive panel of biomarkers – such as the one evaluated in this study – could help to predict those variable paths, paving the way for early interventions to stop or slow the disease.
The authors of the study are affiliated with the WADRC, the Wisconsin Alzheimer’s Institute, the Institute on Aging, the Waisman Center, and the Neuroscience and Public Policy program, all at UW-Madison; and the Geriatrics Research Education and Clinical Center at the William S. Middleton Veterans Hospital.