As imaging and sensing technologies grow in both sophistication and accessibility, they do more than just gather data and produce images:
They are research tools in their own right, providing scientists with the means to deepen our knowledge both about fundamental biological processes and about causes and progression of disease. Obtaining the images is only the first step. Significant research and clinical advances require new ways of analyzing the data.
Current biomedical imaging and sensing technologies include computerized tomography, magnetic resonance imaging, optical coherence tomography, spectroscopy, and ultrasound, to name only a few.
These technologies are at the intersection of the physical sciences, mathematics, computer science, and engineering. Columbia Engineering is home to many imaging and sensing labs, some of which collaborate with labs at Columbia University Medical Center. Our researchers are using biomedical imaging and sensing to study everything from the development of artificial vision systems to bone biomechanics.
Sometimes they work in partnership with technology companies to develop new imaging and sensing techniques. In a constant feedback loop, faculty and researchers pursue technological advances to satisfy unmet scientific and clinical needs; the new technologies then open their eyes to further questions to explore.
Developing Optical Tools for Surgical Guidance
Early in her research career, Christine Hendon was drawn to biomedical optics; she was intrigued by this medical technology that did not rely on radiation. Today, her overall goal is to develop optical tools for surgical guidance.
“We want to develop optical tools that provide the surgeon with a clear understanding of the tissue,” says Hendon, assistant professor of electrical engineering. Her techniques primarily use near-infrared spectroscopy and optical coherence tomography (OCT), which has been dubbed “optical ultrasound.”
So-called optical biopsies would offer much higher resolution than current biopsy surrogates such as MRIs, PET tomography, and ultrasound. A potential advantage of OCT is that the surgeon would be able to image a wide area of tissue and, unlike with invasive biopsies, remove as little tissue as possible.
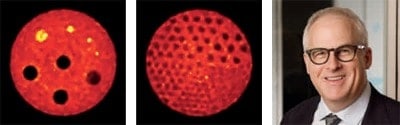
Currently, the main application of Hendon’s research is focusing on OCT in the treatment of heart arrhythmias, or irregular heart rhythms. A common treatment is ablation, in which the surgeon uses a catheter to detect abnormal electrical signals and then applies radiofrequency energy to remove scar tissue in the malfunctioning area.
Hendon is also using spectroscopy to provide real-time information during surgery. Especially important is the depth of a lesion—the ablated, or dead, tissue area. “Frequently,” says Hendon, “patients who have ablation return for a second procedure. We hope that the use of spectroscopy will reduce both procedure time and the number of repeat procedures.”
In late July, Hendon did the first in vivo testing of the spectroscopy catheter on an animal model.
Hendon’s group is building an atlas of OCT heart images. So far, the atlas includes 25 human hearts, with 15 volumes (600 images per volume) for each heart. Eventually, the atlas will be used to train cardiologists.
An upcoming project focuses on the use of optical tools in breast cancer. Hendon is working with breast surgeon Sheldon Feldman and pathologist Hanina Hibshoosh at Columbia University Medical Center to identify tumors localized to the duct. Eventually, they will image lesions over time to determine which are likely to progress to cancer.
Hendon is also collaborating with fellow Columbia Engineering professor Kristin Myers on using imaging to assess the mechanical properties of the cervix in relation to preterm birth.
Hendon is committed to encouraging STEM education among youth. At Columbia, she hosts campus visits by middle-school students—who leave with OCT images of their finger. “Middleschool kids are great,” she said. “They don’t hesitate to ask questions.”
Image Analysis for Both Diagnosis and Treatment Design
In the mid-1980s, Andrew Laine was a graduate student at Washington University, in St. Louis—and a whiz hacker. At the time, the three major manufacturers of medical imaging equipment used different encrypted (proprietary) codes for breast magnetic resonance imaging (MRI) scans. At his adviser’s prompting, Laine cracked the codes, so the data from the various machines could be integrated and the images compared and studied. “Later,” he says, “the federal government ordered imaging manufacturers to adopt a common standard, so images could be shared among VA hospitals.” The result was Digital Imaging and Communications in Medicine (DICOM).
International politics played a role in determining Laine’s next step. With the collapse of the Soviet Union, the U.S. army had a surplus in the defense budget, including $20 million for medical research on women’s diseases. Laine proposed a method to enhance mammograms, to address the problem of visible lesions being overlooked in screening. His technology was ranked the most promising in the program, and he received a $2 million grant for mammography research.
Laine, who is chair of the Department of Biomedical Engineering, with a joint appointment in Radiology at Columbia University Medical Center (CUMC), was the first to apply methods of multiscale “wavelet” representations to enhance subtle details in mammograms so they would not be missed. This not only produced better images, but also reduced the amount of radiation needed for screening. Today, the core algorithm he developed in 1992 is used in almost all commercial digital mammography systems worldwide.
Using a phased array ultrasound transducer, Laine was also the first to compute cardiac strain, which can be a precursor to a heart attack, in real time, from 4D (3D plus time) ultrasound. The 4D imaging can also detect abnormal wall motion of dead myocardial tissue resulting from a heart attack that has already occurred.
“Fostering the relationship between academia and industry,” Laine says, “is the fastest way to bring technical advances in imaging to clinical practice and improve patient care.” Laine spearheaded a partnership between Columbia and General Electric (GE) to foster translational research. It enables biomedical engineers, clinicians, and GE to jointly address unmet clinical needs that could benefit from advances in MRI technology and other imaging methods.
Laine is also applying the wavelet technique he devised for mammography to pulmonary emphysema, a form of chronic obstructive pulmonary disease (COPD). Conventional computed tomography (CT) methods categorize a patient’s disease as one of three subtypes. In collaboration with Graham Barr, MD (CUMC), Laine’s lab is helping to reveal underlying disease stages of COPD by expanding the number of imaging phenotypes used as biomarkers.
By using 3D imaging of CT data and tens of thousands of CT lung scans, and tracking thousands of patients over a decade, Laine has discovered a richer set of 60–80 subtypes of emphysematic tissue.
Laine is also working with Professors George Hripcsak and Larry Schwartz at CUMC. Their research will allow clinicians to study a patient’s history using both text (electronic health record) and annotated findings derived from medical images. This collaboration adds the new dimension of imaging informatics—including radiomics (the extraction and analysis of quantitative features of images)—to precision medicine, furthering our ability to understand disease processes, create new therapies, and better predict patient outcome.