Rutgers neuroscientists have established that problems controlling bodily movements are at the core of autism spectrum disorders and that the use of psychotropic medications to treat autism in children often makes such neuromotor problems worse.
The findings, published recently in Nature Scientific Reports, are contrary to the conventional medical understanding of autism – that it is a mental illness and that neuromotor problems, while often occurring at the same time as autism, are not at its biological core.
“For the first time, we can demonstrate unambiguously that motor issues are core issues that need to be included in the diagnosis criteria for autism,” says Elizabeth Torres, an associate professor of psychology in the School of Arts and Sciences and co-author of the study. Her co-author, Kristina Denisova, a former Rutgers graduate student in psychology, is now an assistant clinical research professor at Columbia University.
According to Torres, psychotropic drugs are routinely prescribed for children on the autism spectrum, even though they’re designed for adults. “Our findings underline the need for clinical trials to determine the effects of these medications on the children’s neuromotor development,” she says. “Doctors should think twice about prescribing such medications for children and parents should insist that they think twice.”
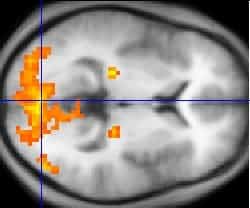
Torres used a new algorithm invented at Rutgers, part of a Statistical Platform for Individualized Behavior Analysis (SPIBA), to analyze the data from functional magnetic resonance imaging (fMRI) scans of 1,048 people, aged 6 to 50, including people with autism spectrum disorders (ASD), and examined the motor patterns as a function of psychotropic medication intake. The resting state fMRI data came from two publicly available databases that Denisova processed to obtain the participants’ involuntary head motions as they tried to lie still in the magnet.
Neuroscientists use fMRI scans to see inside living brains. A patient places his or her head inside an MRI machine, and the machine records several images, or “scans” of the brain. Patients are told to lie still, but inevitably, they move. “Everybody moves,” Torres says. “We can’t help it. Mostly, the movements are involuntary; the clinician can’t see it and the patient isn’t aware of it.”
The MRI machine records the movement, but researchers routinely correct, or “scrub” their scans to eliminate data from involuntary movement. Torres believes that information about the brain gets lost this way, so she and Denisova approached the data differently from other researchers.
“We didn’t start with a hypothesis to test, which is the way this research is usually done,” Torres says. “Instead, we let the data reveal any trends there might be among the subjects we were studying. We asked ourselves, ‘What could these involuntary movements, which researchers usually consider a nuisance, tell us about autism?’”
The data told them that, while everyone moved during fMRI scans and people with autism moved much more, those who were taking psychotropic medicines moved even more than those who were not taking such medicines. “It wasn’t just that they moved more, it was that their patterns worsened over the session,” said Torres. For people with autism taking more than one psychotropic medicine – anti-convulsants and anti-depressants, for example – the amount of movements and the detriment in their patterns were greater still.
“The question is now that we know this, what are we going to do about it?” asks Torres.