The supplement nicotinamide riboside (NR) – a form of vitamin B3 – prevented neurological damage and improved cognitive and physical function in a new mouse model of Alzheimer’s disease. The results of the study, conducted by researchers at the National Institute on Aging (NIA) part of the National Institutes of Health, suggest a potential new target for treating Alzheimer’s disease. The findings appear in the Feb. 5, 2018, issue of Proceedings of the National Academy of Sciences.
NR acts on the brain by normalizing levels of nicotinamide adenine dinucleotide (NAD+), a metabolite vital to cellular energy, stem cell self-renewal, resistance to neuronal stress and DNA repair. In Alzheimer’s disease, the brain’s usual DNA repair activity is impaired, leading to mitochondrial dysfunction, lower neuron production, and increased neuronal dysfunction and inflammation.
“The pursuit of interventions to prevent or delay Alzheimer’s and related dementias is an important national priority,” said Richard J. Hodes, M.D., director of the NIA. “We are encouraging the testing of a variety of new approaches, and this study’s positive results suggest one avenue to pursue further.”
The international team of scientists was led by Vilhelm A. Bohr, M.D., Ph.D., senior investigator and chief of the Laboratory of Molecular Gerontology of the NIA’s Intramural Research Program, with Dr. Yujun Hou, a postdoctoral investigator in the laboratory.
Based on their studies in human postmortem brain, they developed a new strain of mice mimicking major features of human Alzheimer’s such as tau pathology, failing synapses, neuronal death and cognitive impairment. Using this animal model, the researchers tested the effects of an NR supplement by adding it to the drinking water of the mice. Over a three-month period, researchers found that mice who received NR showed reduced tau in their brains, but no change in amyloid-beta.
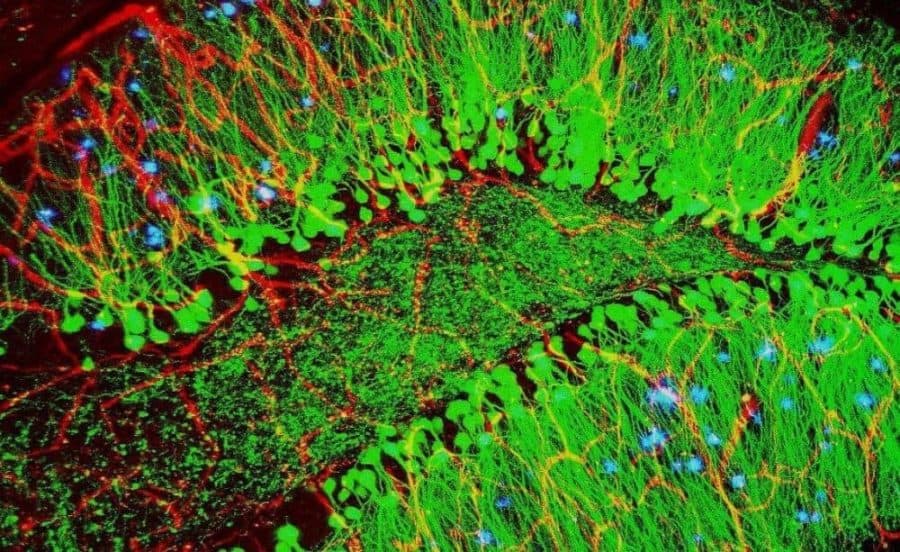
The NR-treated mice also had less DNA damage, higher neuroplasticity (activity and reorganization of brain cells associated with learning or memory), increased production of new neurons from neuronal stem cells, and lower levels of neuronal damage and death. In the hippocampus area of the brain – in which damage and loss of volume is found in people with dementia – NR seemed to either clear existing DNA damage or prevent it from spreading further.
The NR-treated mice also performed better than control mice on multiple behavioral and memory tests, such as water mazes and object recognition. NR mice also showed better muscular and grip strength, higher endurance, and improved gait compared to their control counterparts. The research team believes that these physical and cognitive benefits are due to a rejuvenating effect NR had on stem cells in both muscle and brain tissue.
“We are encouraged by these findings that see an effect in this Alzheimer’s disease model,” said Dr. Bohr. “We are looking forward to further testing of how NR or similar compounds might be pursued for their possible therapeutic benefit for people with dementia.”
Next steps for the research team include further studies on the underlying mechanisms and preparations towards intervention in humans.
The team’s work also included contributions from researchers at the Danish Aging Research Center at the University of Aarhus, and the Center for Healthy Aging at the University of Copenhagen. The Bohr lab has a Cooperative Research and Development Agreement — which allows NIH investigators to join colleagues from industry and academia to pursue common research goals — with ChromaDex Corp.