Much of the research on the underlying causes of Alzheimer’s disease focuses on amyloid beta (Aß), a protein that accumulates in the brain as the disease progresses. Excess Aß proteins form clumps or “plaques” that disrupt communication between brain cells and trigger inflammation, eventually leading to widespread loss of neurons and brain tissue.
Aß plaques will continue to be a major focus for Alzheimer’s researchers. However, new work by neuroscientists at the University of Chicago looks at another process that plays an underappreciated role in the progression of the disease.
In a new study published in the Journal of Neuroscience, Sangram Sisodia, PhD, the Thomas Reynolds Sr. Family Professor of Neurosciences at UChicago, and his colleagues show how in genetic forms of Alzheimer’s, a process called neurogenesis, or the creation of new brain cells, can be disrupted by the brain’s own immune cells.
Some types of early onset, hereditary Alzheimer’s are caused by mutations in two genes called presenilin 1 (PS1) and presenilin 2 (PS2). Previous research has shown that when healthy mice are placed into an “enriched” environment where they can exercise, play and interact with each other, they have a huge increase in new brain cells being created in the hippocampus, part of the brain that is important for memory. But when mice carrying mutations to PS1 and PS2 are placed in an enriched environment, they don’t show the same increase in new brain cells. They also start to show signs of anxiety, a symptom often reported by people with early onset Alzheimer’s.
This led Sisodia to think that something besides genetics had a role to play. He suspected that the process of neurogenesis in mice both with and without Alzheimer’s mutations could also be influenced by other cells that interact with the newly forming brain cells.
Focus on the microglia
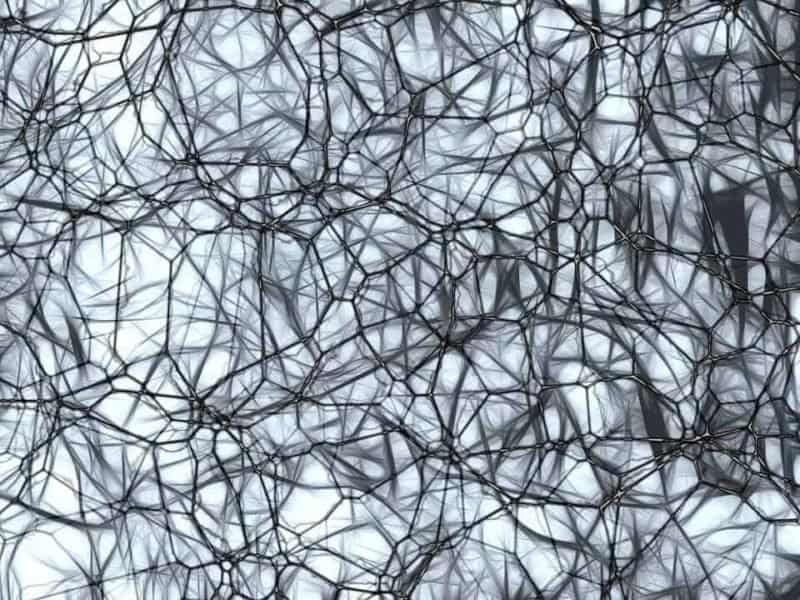
The researchers focused on microglia, a kind of immune cell in the brain that usually repairs synapses, destroys dying cells and clears out excess Aß proteins. When the researchers gave the mice a drug that causes microglial cells to die, neurogenesis returned to normal. The mice with presenilin mutations were then placed into an enriched environment and they were fine; they didn’t show any memory deficits or signs of anxiety, and they were creating the normal, expected number of new neurons.
“It’s the most astounding result to me,” Sisodia said. “Once you wipe out the microglia, all these deficits that you see in these mice with the mutations are completely restored. You get rid of one cell type, and everything is back to normal.”
Sisodia thinks the microglia could be overplaying their immune system role in this case. Alzheimer’s disease normally causes inflammation in the microglia, so when they encounter newly formed brain cells with presenilin mutations they may overreact and kill them off prematurely. He feels that this discovery about the microglia’s role opens another important avenue toward understanding the biology of Alzheimer’s disease.
“I’ve been studying amyloid for 30 years, but there’s something else going on here, and the role of neurogenesis is really underappreciated,” he said. “This is another way to understand the biology of these genes that we know significantly affect the progression of disease and loss of memory.”