In 2020, Alzheimer’s disease was the sixth leading cause of death in the United States. And yet, unlike other leading killers such as heart disease, cancer and stroke, there are currently no effective treatments to prevent or stop it. While deaths from cardiovascular disease declined, deaths from Alzheimer’s more than doubled between 2018 and 2020.
As Americans live longer lives and baby boomers reach their seventies, there is an increasingly desperate need for treatments to prevent Alzheimer’s or slow its symptoms.
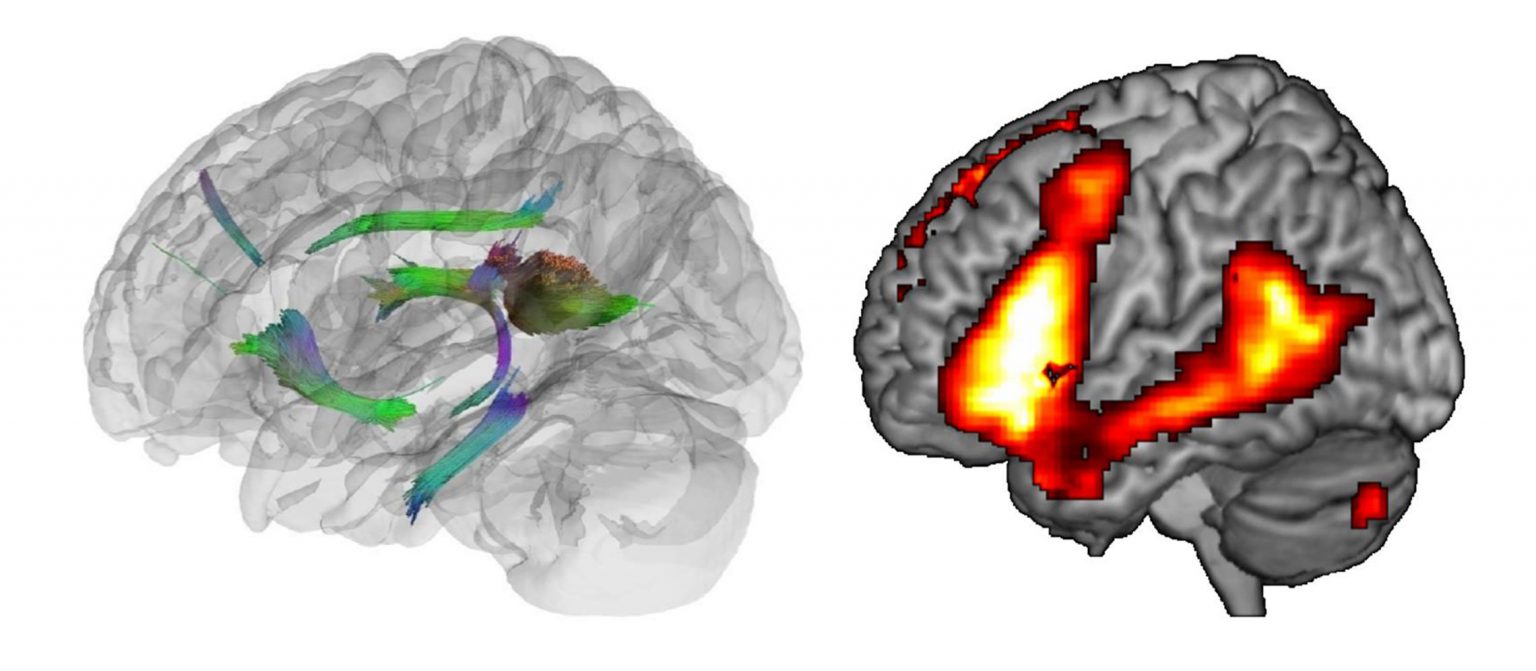
One avenue to discovering improved treatments involves unlocking the secrets of the brain’s natural resilience in the face of injuries, aging and disease. The physical manifestations of Alzheimer’s show up in the brain years before a patient begins having memory problems or other symptoms; somehow the brain compensates for the damage. For some, their brains compensate longer than for others, postponing devastating cognitive loss and personality changes for decades.
Heather Whitson, M.D., professor of medicine, professor of ophthalmology and director of Duke’s Center for Aging and Human Development, has seen many patients who maintain cognitive abilities despite evidence of significant brain pathology. She wonders, “What is the secret? What are their brains doing that we could try to get other people’s brains to do?”
Whitson, a geriatrician, seeks to help people keep their minds and bodies resilient as they age. To that end, she studies lifestyle and environmental factors as well as molecular and cellular processes in the body and brain. She co-directs the Duke-UNC Alzheimer’s Disease Research Collaborative, which brings together Duke and University of North Carolina researchers from multiple disciplines to find ways to prevent or slow the disease, with a special focus on reducing health disparities.
“What is the secret? What are their brains doing that we could try to get other people’s brains to do?”
Heather Whitson
“At the molecular and cellular level, we’ve advanced so much in the past 20 years that I’m hopeful,” she says. Those advances include transcriptomics, which is the ability to measure genetic activity of cells in the lab, as well as new techniques in data science to analyze those measurements. Scientists can take cells from a blood sample, expose them to a stressor — a toxin or a virus, say — and then measure how the genetic machinery in each type of cell responds. Which genes get turned on? Which genes get turned off?
Next, investigators look at how well the person who provided that blood sample is doing in the domain being studied — whether it’s cognition or response to cancer treatment or recovery from surgery. If scientists can identify gene activity that correlates with better real-life outcomes, the next step is to figure out what the gene in question does. If the gene produces a particular protein that has an important job in a particular type of cell, for example, scientists can design pharmaceuticals that would provide that protein to patients, or spur their bodies to produce it.
“We have the opportunity to unlock the resilience of youth,” Whitson says. “And Duke is a really enviable place to be able to do that because of strong programs across our schools of medicine, nursing, and engineering, and our basic sciences. If you look at our peers, you don’t see many that have all of those really highly ranked schools within walking distance. We really benefit from the proximity because it spurs collaboration and promotes team science.”
Whitson also sees great potential in understanding triggers, particularly those related to sensory loss, that may play a role in how Alzheimer’s is diagnosed and how its symptoms progress. As people lose the ability to see, hear or smell, they become more at risk for developing cognitive impairments. “It’s a major stressor to your brain to have less input from your senses,” she says. “I’m trying to understand how the aging brain copes with that.”
Other Duke investigators are looking into additional potential Alzheimer’s triggers, including stressors like metabolic changes, infections and cardiovascular disease — sharing their ideas and insights with others. “It may be a combination of all of these things,” Whitson says.
The fact that brains can cope at all with stressors of this magnitude is due to the brain’s ability to adapt and learn throughout life. “The brain is a learning machine from before birth until death,” says Stephen Lisberger, Ph.D., the George Barth Geller Distinguished Professor for Research in Neurobiology and chair of Duke’s department of neurobiology.
Lisberger studies the very fundamental question of how the brain learns, including how the brain uses experience and visual input to inform movement. “If we can understand that, I think we will reveal general principles that can be applied to [other types of] learning,” he says.
Such general principles could illuminate how the brain adapts to the damage that occurs during the early, pre-symptomatic years of Alzheimer’s disease, and learns ways to compensate for it. Like Whitson, Lisberger believes that understanding how the brain compensates could point to promising pathways for treatment. “If we can understand that resilience, we may be able to harness it as a therapeutic tool,” he says. “Perhaps we can convey resilience to susceptible brains”.
“If you take people at the beginning of their careers and bring them into an environment where collaboration happens and is valued and the expectation is that they will be part of a broader community rather than a silo, then that becomes their culture.”
Stephen Lisberger
Understanding resilience and learning is beyond the ability of any one scientist working in one discipline; it requires a team approach. “Learning [resilience] occurs at so many levels in the brain that it is by its nature a collaborative interdisciplinary effort to understand it,” Lisberger says. As chair, he has intentionally fostered a collaborative environment during the past decade by partnering with other departments across campus, ranging from physics to psychology to cell biology, to hire early-career standout neuroscientists, who approach brain-related questions.
“If you take people at the beginning of their careers and bring them into an environment where collaboration happens and is valued and the expectation is that they will be part of a broader community rather than a silo, then that becomes their culture,” he says. “The kind of collaborative effort we have at Duke is very powerful.”
Lisberger doesn’t know when or how or which research insights will lead to treatment for Alzheimer’s, but he has no doubt it will happen. “I am sure that we will succeed, and the best evidence of that is history,” he says. “Almost every treatment for human disease has come from a serendipitous discovery about how the body works that was made by a basic scientist who was pursuing knowledge for its own sake.”


