Identifying people at high risk for suicide is crucial for applying life-saving interventions and treatments. But it’s hard to know who’s at the greatest risk, and only small improvements have been made in identifying high-risk individuals over the last 50 years. One innovative way to identify people at high risk of suicide is by investigating and identifying brain markers.
Researchers from the VA and BU have found that the functional connectivity between brain networks involved in cognitive control and self-referential thought processing differed among veterans with a history of suicide attempts, even before they tried to end their life – when compared to those with similar levels of psychiatric symptoms, but without a suicide history.
According to corresponding author Audreyana Jagger-Rickels, PhD, principal investigator in the National Centre for PTSD at the VA Boston Healthcare System and assistant professor of psychiatry at Boston University Chobanian & Avedisian School of Medicine, the study provides evidence that this brain connectivity marker may be identifiable before a suicide attempt, suggesting that it could help identify those at risk for suicide. Jagger-Rickels further explained that it could potentially lead to new treatments targeting these brain regions and their underlying functions.
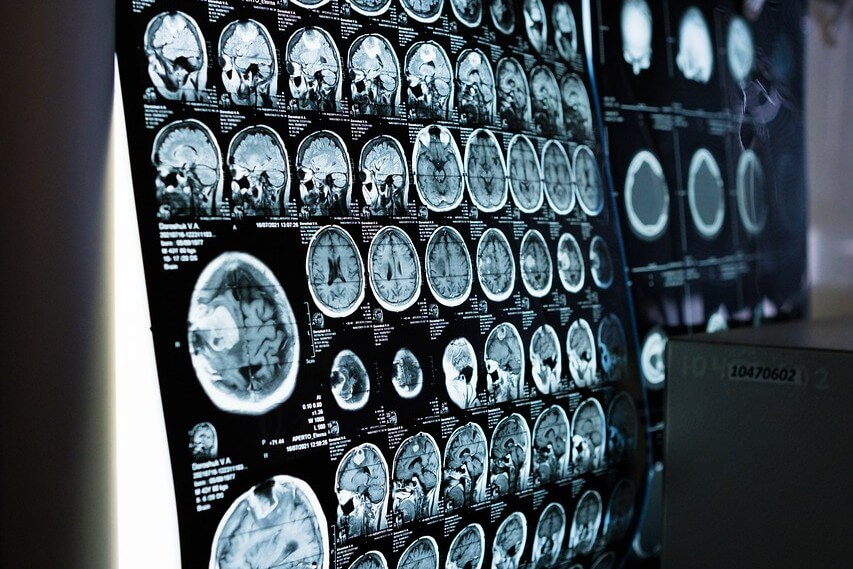
Participants in this study included post-9/11 veterans who participated in a longitudinal study at VA Boston Translational Research Centre for Traumatic Brain Injury and Stress Disorders (TRACTS) that measures brain, cognitive, physical, and psychological health. As part of this study, veterans completed a “resting” functional MRI scan, which measures intrinsic communication between brain regions and networks. From this dataset, they identified a group of veterans who reported a suicide attempt at a one-to-two-year follow-up assessment but who did not report a suicide attempt at any of their previous assessments.
They then identified another group that had equivalent symptoms of depression and post-traumatic stress disorder (PTSD), but did not report a suicide attempt. Having this comparison group allowed the researchers to isolate brain connectivity associated with suicide attempts, rather than other factors like PTSD and depression. They then examined brain connectivity in the suicide attempt group before and after their suicide attempt and compared them to the matched control group. This comparison revealed that brain connectivity between cognitive control and self-referential processing networks was dysregulated in the suicide attempt group. Critically, this brain connectivity signature of suicide risk was present both before and after the attempt, suggesting that this brain marker may be a novel suicide-specific risk factor.
One of the challenges in suicide risk assessment is that it primarily relies on the method of self-reporting. Jagger-Rickels explained that interventions to reduce suicide risk are limited to people who feel comfortable enough to disclose (self-report) suicidal thoughts and behaviours. Identifying measures that do not require self-disclosure of suicidal thoughts and behaviours may help identify people who are overlooked and may also aid in the development of novel treatments targeting the brain mechanisms underlying suicidal thoughts and behaviours.
The study also indicated that connectivity of the right amygdala, a brain region important for fear learning and trauma, differed between the suicide attempt group and the matched control group, but only after reporting a suicide attempt. This suggests that there are brain changes that occur after a suicide attempt, which could be related to the stressors surrounding a suicide attempt or due to the trauma of the suicide attempt itself. This would indicate that suicide attempts themselves impact the brain, which could increase future suicide risk.
These findings appear online in the Journal of Affective Disorders.