Columbia researchers have identified brain injuries that may underlie hidden consciousness, a puzzling phenomenon in which brain-injured patients are unable to respond to simple commands, making them appear unconscious despite having some level of awareness.
“Our study suggests that patients with hidden consciousness can hear and comprehend verbal commands, but they cannot carry out those commands because of injuries in brain circuits that relay instructions from the brain to the muscles,” says study leader Jan Claassen, MD, associate professor of neurology at Columbia University Vagelos College of Physicians and Surgeons and chief of critical care and hospitalist neurology at NewYork-Presbyterian/Columbia University Irving Medical Center.
The findings could help physicians more quickly identify brain-injured patients who might have hidden consciousness and better predict which patients are likely to recover with rehabilitation.
Brain circuits disrupted in patients with hidden consciousness
Hidden consciousness, also known as cognitive motor dissociation (CMD), occurs in about 15% to 25% of patients with brain injuries stemming from head trauma, brain hemorrhage, or cardiac arrest.
In previous research, Claassen and colleagues found that subtle brainwaves detectable with EEG are the strongest predictor of hidden consciousness and eventual recovery for unresponsive brain-injured patients.
But the precise pathways in the brain that become disrupted in this condition were unknown.
In the new study, the researchers used EEG to examine 107 brain injury patients. The technique can determine when patients are trying, though unable, to respond to a command such as “keep opening and closing your right hand.”
The analysis detected CMD in 21 of the patients.
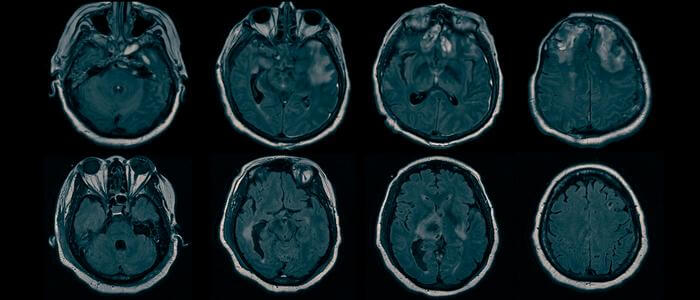
The researchers then analyzed structural MRI scans from all of the patients.
“Using a technique we developed called bi-clustering analysis, we were able to identify patterns of brain injury that are shared among patients with CMD and contrast to those without CMD,” says co-lead author Qi Shen, PhD, associate research scientist in the Claassen lab and an expert in signal processing, machine learning, and biostatistics.
The researchers found that all of the CMD patients had intact brain structures related to arousal and command comprehension, supporting the notion that these patients were hearing and understanding the commands but were unable to carry them out.
“We saw that all of the CMD patients had deficits in brain regions responsible for integrating comprehended motor commands with motor output, preventing CMD patients from acting on verbal commands,” says Claassen.
The findings may allow researchers to better understand which brain injury patients have CMD, which will be useful for clinical trials that support recovery of consciousness.
More research is required before these approaches can be applied to clinical practice. “However, our study shows that it may be possible to screen for hidden consciousness using widely available structural brain imaging, moving the detection of CMD one step closer to general clinical use,” Claassen says.
“Not every critical care unit may have resources and staff that is trained in using EEG to detect hidden consciousness, so MRI may offer a simple way to identify patients who require further screening and diagnosis.”
More information
The study, titled “Injury patterns associated with cognitive motor dissociation,” was published online in the journal Brain.
All authors: Eva Franzova (Columbia), Qi Shen (Columbia), Kevin Doyle (Columbia), Justine M. Chen (Columbia), Jennifer Egbebike (Columbia), Athina Vrosgou (Columbia), Jerina C. Carmona (Columbia), Lauren Grobois (Columbia), Gregory A. Heinonen (Columbia), Angela Velazquez (Columbia), Ian Jerome Gonzales (Columbia and NewYork-Presbyterian), Satoshi Egawa (Columbia and NewYork-Presbyterian), Sachin Agarwal (Columbia and NewYork-Presbyterian), David Roh (Columbia and NewYork-Presbyterian), Soojin Park (Columbia and NewYork-Presbyterian), E. Sander Connolly (Columbia and NewYork-Presbyterian), and Jan Claassen (Columbia and NewYork-Presbyterian).
The study was supported by grants from the National Institutes of Health (R01NS106014 and R03NS112760) and the Dana Foundation.
The authors report no competing interests.