A groundbreaking study from the University of California San Diego has revealed that an experimental cancer drug could potentially enhance cognitive function in individuals with Rett syndrome, a rare disorder associated with autism. This discovery opens new avenues for treating various neurological conditions by targeting microglia, the brain’s immune cells.
Unveiling the Role of Microglia in Brain Development
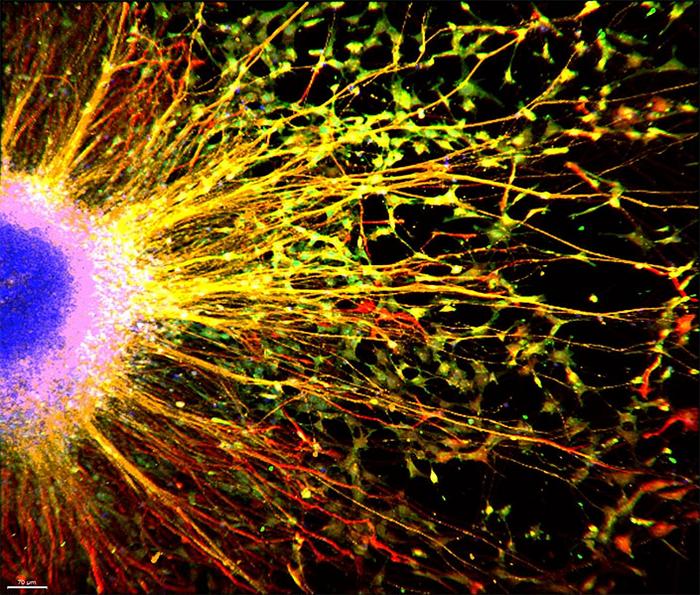
Researchers used brain organoids – miniature lab-grown brain models – to investigate the function of microglia in early neural development. By adding healthy microglia to organoids derived from Rett syndrome patients, they observed a remarkable improvement in synaptic function.
Dr. Pinar Mesci, the study’s lead researcher, explained: “We found that introducing healthy microglia to Rett syndrome brain organoids rescued synaptic functioning by restoring phagocytosis, a crucial process for maintaining brain health.”
Phagocytosis allows microglia to remove foreign substances and prune unnecessary synapses, optimizing brain function. In Rett syndrome, this process is impaired due to a loss of function in the MECP2 gene.
ADH-503: A Potential Game-Changer for Neurological Disorders
The team screened existing drugs to find one that could restore microglia function. They identified ADH-503, an experimental oral pancreatic cancer medication, as a promising candidate.
ADH-503 regulates CD11b, a protein involved in phagocytosis. By improving microglia function, the drug could potentially ease cognitive difficulties for Rett syndrome patients and those with other neurological conditions.
Professor Alysson Muotri, senior author of the study, noted: “If the brain’s ‘janitors’ are not working, problems start to arise. By focusing on improving how microglia function, we might create a better environment for neurons and ease functioning for patients.”
Why it matters: This research represents a significant step forward in understanding and potentially treating Rett syndrome and other neurodevelopmental disorders. By targeting microglia rather than neurons, the approach offers hope for improving cognitive function even after diagnosis.
The study, published in Stem Cell Reports, marks the first successful integration of human microglia into Rett syndrome brain tissues in vitro. This model may prove superior to traditional mouse models for studying the disorder.
Dr. Jonathan Kipnis, an expert in neuroimmunology at Washington University School of Medicine, praised the study: “This work nicely demonstrates microglia as a potential therapeutic target in Rett syndrome. Understanding neuro-immune interactions in this complex disease may not only provide new insights into the disease biology but also develop novel approaches to attenuate its progression.”
As researchers continue to explore the potential of ADH-503 and similar compounds, there is growing optimism about developing therapies that could improve quality of life for individuals with Rett syndrome and other neurological disorders.