Researchers have created the largest collection of stem cell models from multiple sclerosis (MS) patients to date, revealing new insights into the disease. The study, published in Cell Stem Cell, highlights the unexpected role of glial cells in MS progression, potentially opening doors for novel treatment approaches.
Glial Cells: The Unsung Players in MS
A team of scientists from The New York Stem Cell Foundation (NYSCF) Research Institute and Case Western Reserve University has made a significant discovery in MS research. They found that glial cells, which support and protect neurons in the brain, show signs of disease even without the influence of the immune system.
Dr. Valentina Fossati, NYSCF Senior Research Investigator and lead author of the study, explained: “Most research and therapeutic strategies have so far focused on blocking the overactive immune system, but how cells in the brain itself, especially glia, contribute to the initiation and progression of MS remained a mystery.”
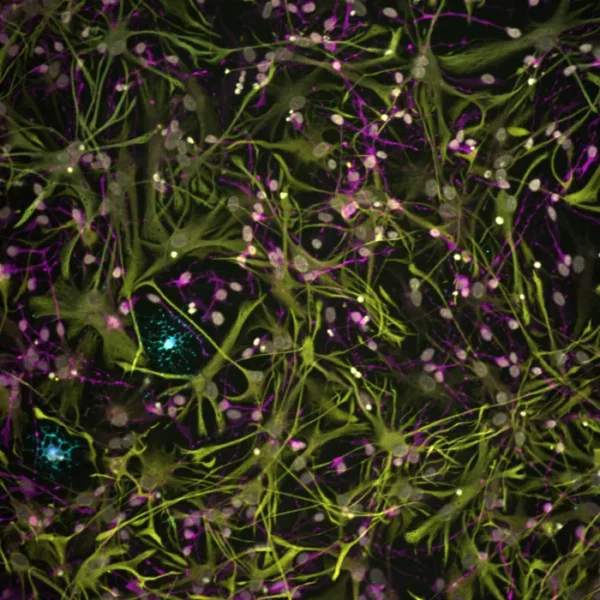
The researchers used induced pluripotent stem cells (iPSCs) created from skin biopsies of MS patients to generate glial cells, including oligodendrocytes and astrocytes. This approach allowed them to study these cells in isolation from the complex environment of the body.
Challenging Conventional Understanding
Using advanced techniques like single-cell gene expression profiling, the team made several key discoveries:
- Stem cell-derived glial cultures from patients with primary progressive MS (a severe form of the disease) contained fewer oligodendrocytes, which are responsible for producing the protective myelin sheath around nerve fibers.
- Genes associated with immune and inflammatory functions were particularly active in stem cell-derived glial cultures from MS patients, mirroring observations in brain samples from deceased MS patients.
- Artificial intelligence detected subtle differences in astrocytes that are not easily seen by the human eye.
Dr. Paul Tesar, co-lead of the study and professor at Case Western Reserve University School of Medicine, noted: “This observation challenges the conventional understanding of MS as being purely driven by immune system dysfunction, suggesting that the disease may also be fueled by processes originating within the brain itself.”
Why It Matters
These findings have significant implications for MS treatment:
- Current therapies primarily target the immune system, reducing the frequency of attacks but falling short in preventing neurodegeneration.
- The discovery of glial cell involvement opens up new possibilities for treatments that directly target these cells.
- This approach could lead to more effective therapies that address both the immune and neurological aspects of MS.
Dr. Tesar emphasized the potential impact: “Our findings represent a significant leap forward in our understanding of MS and underscore the vast potential in glia as a target for therapeutic intervention that could transform the treatment landscape for many patients.”
A New Frontier in MS Research
This study represents a major advancement in MS research, made possible by the combination of NYSCF’s large-scale stem cell modeling capabilities and the Tesar lab’s expertise in glial cell biology. The research team included collaborators from the Corinne Goldsmith Dickinson Center for Multiple Sclerosis and the CUNY Graduate Center.
Jennifer J. Raab, NYSCF’s President and CEO, highlighted the importance of collaboration: “This study is a remarkable example of team science. It is through unique collaborations like these that we can move even faster towards new treatments for the major diseases of our time that patients urgently need.”
The study’s findings raise several questions for future research:
- How do glial cell abnormalities interact with immune system dysfunction in MS?
- Can targeting glial cells lead to more effective treatments for progressive forms of MS?
- Are there potential biomarkers in glial cells that could help diagnose MS earlier or predict disease progression?
As researchers continue to explore these questions, the stem cell models developed in this study provide a valuable resource for further investigations into MS and other neurological disorders.