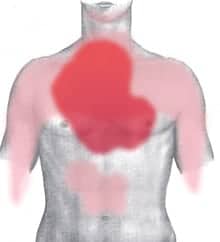
For women taking certain kinds of pain relievers, a heart attack could be waiting in their medicine cabinets.
A University of Florida study has found that the regular use of some non-steroidal anti-inflammatory drugs, or NSAIDs, increases the risk of stroke, heart attack and death in postmenopausal women. The study was published this week in the journal Circulation: Cardiovascular Quality and Outcomes.
The researchers found that regular use of the NSAID naproxen, the active ingredient in medications such as Aleve, is associated with a 10 percent increased risk of heart attack, stroke and death in postmenopausal women, said UF cardiologist Dr. Anthony Bavry, the study’s lead author. Regular use was defined as at least twice per week for the previous two weeks.
“That is counter to the medical community’s perception of NSAIDs, in which most people believe naproxen to be safer,” Bavry said. “Our study showed naproxen was not safer — it was actually harmful.”
Bavry, in collaboration with researchers from Harvard and other universities, combed through data from more than 160,000 postmenopausal women who were surveyed as part of the Women’s Health Initiative — a 15-year research study funded by the National Institutes of Health. Of these women, 53,142 regularly used NSAIDs. Even after controlling for obesity, hypertension, diabetes, use of aspirin and other health factors, the researchers found the increased risk for heart attack, stroke or death among the women who used certain types of NSAIDs.
One of the study’s co-authors, Dr. Marian Limacher, has been the UF principal investigator for the Women’s Health Initiative since 1994. She emphasized that the study was observational in nature, which helped the researchers find associations between use of NSAIDs and cardiovascular impacts. Limacher also noted that this was the first study of its size to examine the effects of regular NSAID use on women.
“When we study agents such as aspirin, we have found differential effects in men and women,” Limacher said. “Men had reduction in heart attack, and older women had a reduction in stroke but not heart attack, which is part of the reason those of us studying women feel we really need to have adequate information on commonly used drugs for both men and women,”
NSAIDs include over-the-counter medications such as naproxen and ibuprofen as well as prescription drugs such as rofecoxib, commercially branded as Vioxx, and celecoxib, branded as Celebrex. Because of its association with increased risk of heart attack or stroke, Vioxx was taken off the market in 2004.
The study’s main finding confirmed that the regular use of any NSAID was associated with harm such as digestive bleeding. Although it found for the first time that the risk of heart attack, stroke or death was associated with the use of naproxen, the study found no cardiovascular or stroke harm associated with ibuprofen.
NSAIDs work by inhibiting two enzymes responsible for inflammation, called cox-1 and cox-2. They also can cause bleeding in the stomach and digestive tract. NSAIDs that target just the cox-2 enzyme, which is present mainly at the site of inflammation, are designed to prevent bleeding in the digestive tract, Bavry said.
However, previous studies showed that NSAIDs that solely target the cox-2 enzyme, which include Vioxx and Celebrex, have been associated with adverse cardiovascular events such as heart attack or stroke. Bavry thinks the culprit in naproxen is also cox-2 inhibition.
“People will have to think about what they have in their own medicine cabinet,” Bavry said. “Do they have naproxen, ibuprofen or something else?”
The study looked only at the association between cardiovascular events and use of NSAIDs — not the effects of NSAIDs on the kidneys, for example.
“We would encourage patients to use medications for as short a time as they need, and to be sure they follow up with their physicians regularly to monitor for effects on the kidneys, and potentially for risk for heart disease,” Limacher said.