The pathological process amyloidosis, in which misfolded proteins (amyloids) form insoluble fibril deposits, occurs in many diseases, including Alzheimer disease (AD) and type 2 diabetes mellitus (T2D). However, little is known about whether different forms of amyloid proteins interact or how amyloid formation begins in vivo. A study published in The American Journal of Pathology has found evidence that amyloid from the brain can stimulate the growth of fibrils in the murine pancreas and pancreatic-related amyloid can be found along with brain-related amyloid in human brain senile plaques.
Islet amyloid can be found in islets of Langerhans in almost all patients with T2D. Islet amyloid is made up of islet amyloid polypeptide (IAPP), which is derived from its precursor proIAPP. Accumulation of IAPP can lead to beta-cell death. In the brain, deposits of beta-amyloid in the cortex and blood vessels are characteristic findings in AD.
Several clinical studies have shown that patients with T2D have almost a two-fold greater risk of developing AD. The data described in the current study suggest that one link between the two diseases may be the processes underlying amyloidosis.
This investigation focused on understanding how amyloid deposits “seed” or spread within a tissue or from one organ to another. “Several soluble proteins are amyloid forming in humans. Independent of protein origin, the fibrils produced are morphologically similar,” said Gunilla T. Westermark, PhD, Department of Medical Cell Biology at Uppsala University (Sweden). “There is a potential for structures with amyloid-seeding ability to induce both homologous and heterologous fibril growth. Heterologous seeding between IAPP and beta-amyloid may represent a molecular link between AD and T2D.” [Homologous fibril growth refers to the growth of fibrils from the same protein. Heterologous fibril growth is when fibrils from one amyloid-forming protein stimulate the growth of fibrils from a different amyloid protein.]
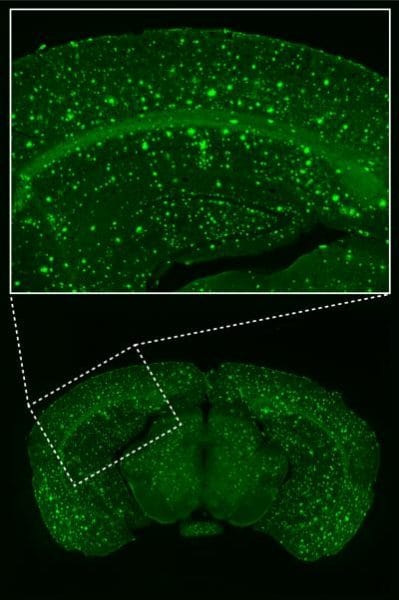
Researchers first injected transgenic mice expressing human IAPP with preformed fibrils of synthetic IAPP, proIAPP, or beta-amyloid. After 10 months on a high-fat diet, tissue was analyzed using an amyloid-specific dye. The number of islets with amyloid was significantly increased compared to controls by all three types of fibrils, and the amyloid consisted of IAPP in all groups. No amyloid deposits were found in the spleen, kidney, liver, heart, or lungs. The results demonstrate for the first time that fibril injections could seed amyloid formation in the pancreas and also that brain amyloid could cross-seed fibril formation in the pancreas.
In subsequent experiments the investigators analyzed human tissues from the pancreas and brain. Using antibody-based methods, they found that pancreas sections with islet amyloid from patients diagnosed with T2D showed no beta-amyloid immunoreactivity, whereas all samples were immunoreactive for IAPP.
To further investigate whether IAPP and beta-amyloid co-localize in human brain tissue researchers analyzed samples from the temporal cortex from AD patients and age-matched non-AD patients with frontotemporal dementia, progressive supranuclear palsy (PSP), or no neurological diagnosis. They found IAPP reactivity in all samples analyzed. In fact, AD samples contained 1.4-times higher IAPP concentrations than samples from non-AD patients.
“It is not clear if IAPP found in brain is locally produced or derived from pancreatic beta-cells,” commented Dr. Westermark. “Cross-seeding by other amyloid aggregates or perhaps by other types of aggregates offers one possible mechanism for initiation of amyloid formation. Interactions between amyloid and other aggregation-prone proteins may be of great importance in the development of protein-misfolding diseases.”