For much of her adult life Valerie Sim has been fascinated by a disease very few in the world can claim to even begin to understand. Sim is one of Canada’s foremost authorities on prion disease–more commonly known as bovine spongiform encephalopathy, or mad cow disease in cattle, or Creutzfeldt-Jacob disease among humans. In both cases there is no cure; nor are there treatments available. But Sim’s latest research is providing new hope for the future.
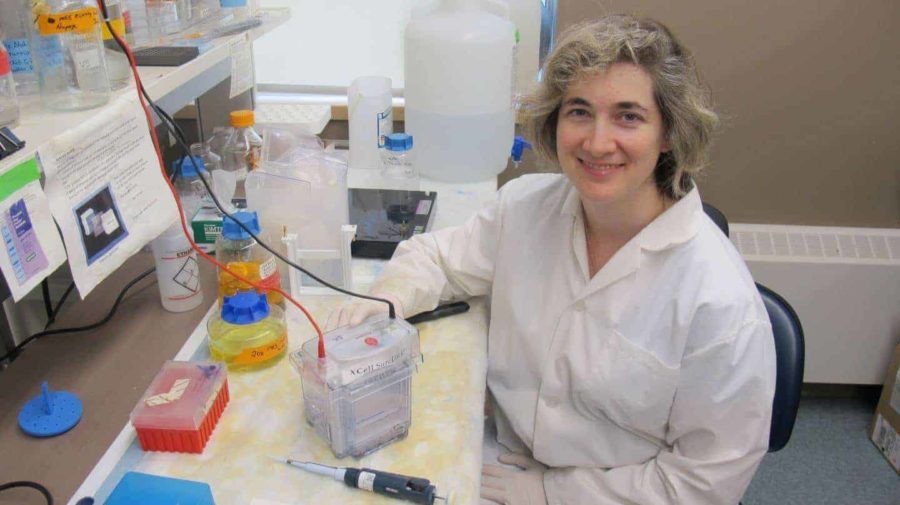
Sim, an assistant professor in the University of Alberta’s Faculty of Medicine & Dentistry, and Leonardo Cortez, a research associate in her lab, are the main authors of a study in the August issue of the Journal of Virology examining the use of two bile acids as possible therapeutic treatments for prion disease. The research found that ursodeoxycholic acid (UDCA) and tauroursodeoxycholic acid (TUDCA) helped slow the progression of the disease if given early in the disease process. The bile acids appear to bind the proteins (prions) that cause disease and prevent them from spreading.
“These compounds are normally used to help digest lipids and fats, but interestingly they’ve been used in naturopathic and Chinese remedies for hundreds of years,” says Sim. “Right now we have nothing to offer patients with prion disease. This could be a way forward.”
Creutzfeldt-Jacob disease is rare in humans, affecting approximately one person out of every million. It is a fatal neurodegenerative disease caused when a protein in the brain takes on a wrong shape, which then converts other proteins to misfold as well. When that occurs, it begins a tremendously accelerated type of dementia, affecting a person’s memory, coordination, vision and balance. While most cases are sporadic and unpredictable, in about 10 per cent of all cases the disease is actually inherited. In extremely rare cases it can also be transmitted through eating contaminated meat.
While Sim’s research marks important new progress, she cautions it needs further study in humans. She also notes that the use of UDCA and TUDCA would not be effective in most cases of prion disease as patients only come to medical attention after the disease is already too far progressed. She does believe the findings could have application for the 10 per cent of Creutzfeldt-Jacob patients who have a genetic form of the disease and who could seek early long-term treatment.
“Some of those people know they are carriers of the disease and currently we have nothing we can give them that works,” says Sim. “This is not a cure, but may have some benefit if given early. And for these patients, any benefit is better than nothing.”
With possible clinical applications still years away, Sim and her team are continuing their research. They hope to learn if UDCA and TUDCA would have long-term health benefits for patients with prion disease, or if it would simply extend life at the end stage of the disease when symptoms are at their worst. They are also testing to see if they can boost the effectiveness of UDCA and TUDCA by combining them with other anti-prion compounds.
While work continues on the research, Sim says there are still common sense solutions that can be taken in the meantime to keep the brain functioning at its best.
“I wouldn’t propose going out and adding bile acids to the water in an attempt to prevent such a rare disease,” she says. “For now, the best ways to reduce the risk of the more common dementias are to stop smoking, exercise, eat well, and get a healthy night’s sleep. These are much better for the brain.”
Research funding was provided by Alberta Innovates – Bio Solutions, Alberta Innovates – Health Solutions, and the University Hospital Foundation.