Mutant forms of breast cancer factor 1 (BRCA1) are associated with breast and ovarian cancers but according to new findings, in the brain the normal BRCA1 gene product may also be linked to Alzheimer’s disease. The results, published in Nature Communications, suggest that low levels of BRCA1 protein in the brain may contribute to dementia. The study was funded by the National Institutes of Health.
“It’s extremely interesting that one molecule can be critically involved in two apparently opposing conditions: cancer, in which too many cells are born and neurodegenerative disease, in which too many brain cells die off,” said senior author Lennart Mucke, M.D., director of the Gladstone Institute of Neurological Disease, San Francisco, and the Joseph B. Martin Distinguished Professor of Neuroscience, and professor of neurology at the University of California, San Francisco.
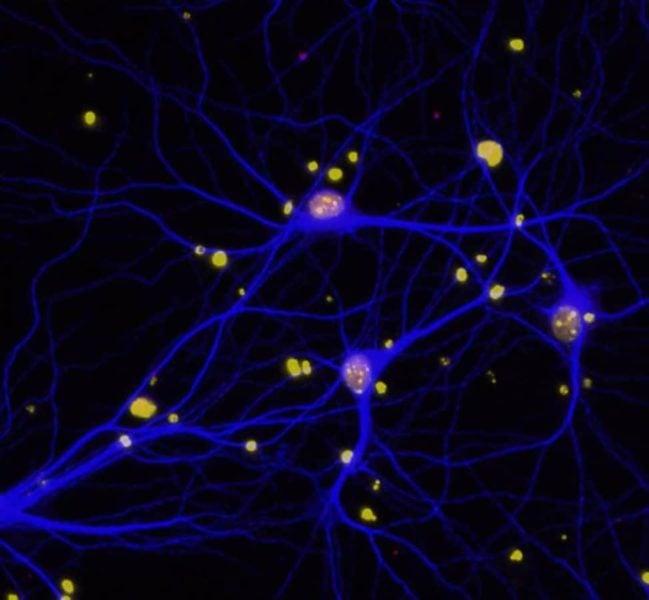
Dr. Mucke and his colleagues suspected that defects in DNA repair mechanisms could contribute to cognitive decline in AD and focused their studies on BRCA1. BRCA1 plays a key role in repairing deoxyribonucleic acid (DNA), our genetic code. DNA is a double helix structure that is made of two strands and resembles a twisted ladder. Occasionally, one or both of the strands will develop breaks, which are fixed by DNA repair proteins including BRCA1. This process is critical for cell survival because if DNA is not repaired properly, the cell may die.
When Dr. Mucke’s group examined brains of patients who died with Alzheimer’s, they discovered low levels of BRCA1. In addition, the researchers found reductions of BRCA1 in the brains of mouse models of Alzheimer’s. In fact, experimental reduction of BRCA1 levels in brains of healthy mice made their brain cells shrink and become dysfunctional.
Dr. Mucke’s team also investigated the effects of BRCA1 on cognition. After researchers reduced BRCA1 levels in the brains of healthy mice, the animals developed problems with learning and memory. Mouse models of Alzheimer’s showed even greater declines in learning and memory following reductions of BRCA1. In addition, lowering BRCA1 caused increased DNA damage in the brains of Alzheimer’s mice.
One of the hallmarks of Alzheimer’s disease is accumulation of a protein fragment known as beta-amyloid, which is toxic to brain cells and can lead to neuronal death. Dr. Mucke’s team found that adding amyloid beta to neurons in a dish lowered levels of BRCA1.
According to Dr. Mucke and his colleagues, the findings suggest that accumulation of beta-amyloid lowers levels of BRCA1, which increases DNA damage in brain cells and may contribute to dementia.
“An emerging theme in neurodegeneration research is that normal DNA repair protects against damage that causes neurons to die in dementia and related disorders. This study supports and strengthens that theme by showing that beta-amyloid decreases the levels of the DNA repair gene BRCA1, and at the same time inhibits the ability to form new memories,” said Roderick Corriveau, Ph.D., program director at NIH’s National Institute of Neurological Disorders and Stroke, which provided funding for the study.
“The functions of BRCA1 in the brain remain to be fully elucidated,” said Dr. Mucke, “but our findings suggest that it may play an important role in supporting critical brain functions in both health and disease.”
Further research is necessary to determine whether BRCA1 may be a potential therapeutic target for treating dementia, and whether BRCA1 mutations that lead to cancer also affect brain function.
The NINDS is the nation’s leading funder of research on the brain and nervous system. The mission of NINDS is to seek fundamental knowledge about the brain and nervous system and to use that knowledge to reduce the burden of neurological disease.