A common theme in medicine is that detecting a disease early on can lead to more effective treatments. This relies partly on luck that the patient gets screened at the right time, but more important is that the testing techniques are sensitive enough to register the minuscule hints that diseases leave in the blood stream.
A new technique developed by a team of chemists at Stanford has shown promise to be thousands of times more sensitive than current techniques in lab experiments, and it is now being put to test in real-world clinical trials.
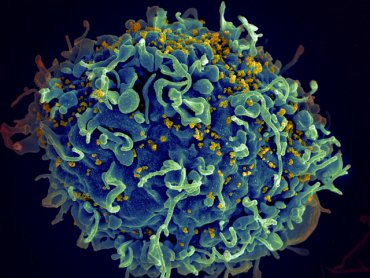
When a disease – whether it’s a cancer or a virus like HIV – begins growing in the body, the immune system responds by producing antibodies. Fishing these antibodies or related biomarkers out of the blood is one way that scientists infer the presence of a disease. This involves designing a molecule that the biomarker will bind to, and which is adorned with an identifying “flag.” Through a series of specialized chemical reactions, known as an immunoassay, researchers can isolate that flag, and the biomarker bound to it, to provide a proxy measurement of the disease.
The new technique, developed in the lab of Carolyn Bertozzi, a professor of chemistry at Stanford, augments this standard procedure with powerful DNA screening technology. In this case, the chemists have replaced the standard flag with a short strand of DNA, which can then be teased out of the sample using DNA isolation technologies that are far more sensitive than those possible for traditional antibody detections.
“This is spiritually related to a basic science tool we were developing to detect protein modifications, but we realized that the core principles were pretty straightforward and that the approach might be better served as a diagnostic tool,” said Peter Robinson, a co-author on the study and graduate student in Bertozzi’s group.
The researchers tested their technique, with its signature DNA flag, against four commercially available, FDA-approved tests for a biomarker for thyroid cancer. It outperformed the sensitivity of all of them, by at least 800 times, and as much as 10,000 times. By detecting the biomarkers of disease at lower concentrations, physicians could theoretically catch diseases far earlier in their progression.
“The thyroid cancer test has historically been a fairly challenging immunoassay, because it produces a lot of false positives and false negatives, so it wasn’t clear if our test would have an advantage,” Robinson said. “We suspected ours would be more sensitive, but we were pleasantly surprised by the magnitude.”
Putting basic research to use in a clinical setting has been a focus of Bertozzi’s since she arrived at Stanford.
“I moved to Stanford with the anticipation that translation of my students’ innovations to clinically impactful products and technologies would be enabled,” said Bertozzi, who is a faculty fellow of Stanford ChEM-H, as well as a professor, by courtesy, of radiology and of chemical and systems biology. “That goal is being delightfully fulfilled.”
Based on the success of the thyroid screening, the group has won a few grants to advance the technique into clinical trials. One trial underway in collaboration with the nearby Alameda County Public Health Laboratory will help evaluate the technique as a screening tool for HIV. Early detection and treatment of the virus can help ensure that its effects on the patient are minimized and reduce the chance that it is transmitted to others. This effort is supported by a pilot grant from Stanford-Spectrum, funded by the National Center for Advancing Translational Sciences at the National Institutes of Health.
“Many of our collaborators are excited that the test can be readily deployed in their lab,” said co-author Cheng-ting “Jason” Tsai, a graduate student in Bertozzi’s group. “In contrast to many new diagnostic techniques, this test is performed on pre-existing machines that most clinical labs are already familiar with.”
The researchers are also pursuing tests for Type 1 diabetes, for which early detection could help patients manage the disease with fewer side effects.