When the first heat wave of summer arrives, a grim tally will start: the number of people who die as a result.
According to the Centers for Disease Control, we can expect high temperatures to kill nearly 700 people each year in this country alone, most of them over 70 years of age. The vast majority won’t die of heat stroke, heat exhaustion, or dehydration. They will die of heart-related problems, including heart attacks and heart failure.
The reason, says Penn State physiologist Larry Kenney, is that we cool ourselves largely by pumping more blood to the skin, where the heat it carries can be lost to the environment. During hot weather, the increase in blood flow to the skin is huge, up to 20 times as much as in cooler weather. Even at rest, if we’re very hot, we may be pumping nearly two gallons of blood to our skin every minute.
High temperatures kill nearly 700 people each year in this country alone, most of them over 70 years of age.
That creates a strain on the heart that can be a particular problem for older people, as their hearts work harder trying to pump more blood to the skin. To make matters worse, the blood vessels in older skin don’t dilate as well as the vessels in the skin of younger people. They can’t accommodate the greater flow and can’t return as much blood to the heart.
“It’s kind of a double-whammy,” says Kenney. “Older adults don’t pump as much blood to the skin, but the left ventricle is still trying to contract very forcefully to do that. So in some older individuals who have heart failure, who had had a heart attack, or who just have a weak left ventricle, all of a sudden they’re putting much more stress on the heart”—sometimes with disastrous results.
Sweating the details
Kenney has worked on the effects of age on temperature regulation since 1983, when he received his first National Institutes of Health grant for the research. Initially he focused on sweating.
“There was an old notion that as people age, sweat glands actually atrophy and don’t function anymore—that the elderly don’t produce as much sweat. That would lead to less evaporative cooling,” he says.
His lab found that while we do tend to sweat less as we age, that’s only partly due to age-related changes in the glands. It’s also due to changes in our activities.
“Sweating as a means of thermoregulation is much more affected by aerobic fitness level, how acclimated you are to the heat, how well hydrated you are, whether you have a sedentary lifestyle, et cetera,” he says—things that often accompany aging but are not directly caused by aging.
Those early studies showed, however, that the ability to lose heat through our skin is directly related to age.
“While sweating is not always directly related to how old we are, the ability to constrict and dilate the blood vessels in the skin really is,” says Kenney. “So for the past 15 years or so, we’ve focused on that aspect of temperature regulation.”
Uniquely human
Human skin responds rapidly and precisely to changes in both heat and cold, with tiny vessels called arterioles dilating or constricting to help dissipate heat or conserve it. The mechanisms that allow humans to achieve this precise control, and the magnitude of changes in skin blood flow, set us apart from our nearest relatives as much as walking upright and having opposable thumbs.
“It’s a uniquely human system,” says Kenney. “There’s not any other animal that regulates their skin blood flow the way humans do.” Some other mammals change the flow of blood to their skin, but by completely different mechanisms and often only in certain parts of the body. Rats control blood flow to their tails; rabbits change blood flow to their ears. But only humans increase skin blood flow over their whole bodies, and by such a large amount.
“There’s not any other animal that regulates their skin blood flow the way humans do.”
The rise in skin blood flow can be so dramatic that it increases the diameter of our limbs enough that Kenney can measure it with a strain gauge wrapped around a forearm. “It’s very subtle,” he says. “It’s in the fractions of a percent change in circumference of the strain gauge—but the more blood that flows to that forearm, the more the strain gauge stretches.”
In recent years, his lab has turned to laser techniques to more precisely measure blood flow in the skin. With laser Doppler flowmetry, a researcher shines a laser into an area of skin about the diameter of a pencil. Red blood cells flowing through tiny vessels there reflect the light. The amount of change in the reflection indicates how many red blood cells are moving through the area.
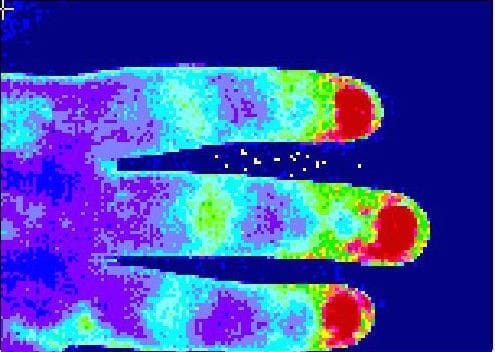
Another technique, laser speckle imaging, uses dots, or speckles, of reflected laser light to show relative changes in blood flow across a larger area of skin—an entire hand or foot, for example. “All pictures are made of speckles,” Kenney says—think of pixels on a computer screen. “If it’s a biological tissue, those speckles move and change, and they change with blood flow.” He uses a special camera to track that movement in real time. In the resulting images, the speckles are color-coded to indicate how many of them were moving in each portion of the image. Areas of dilation (more flow) show up bright red and yellow, while areas where the vessels were constricted (less flow) are a calm dark blue.
Cool tools
Because these large changes in skin blood flow and the molecular mechanisms that control them are unique to humans, Kenney can’t use mice or other lab animals for his studies. He relies on human volunteers willing to be heated up or cooled down while exercising or going through other experimental approaches. For his experiments, the “older” category starts at age 65; some of his volunteers are in their 90s.
Volunteers often recline or sit, and can watch movies (comedies, mostly), read, or just hang out—unless they’re in one of the studies looking at how well they dissipate heat generated by exercise. In that case, they sit or recline on a clinical bed outfitted with pedals, something like a recumbent bicycle, or walk or jog on a treadmill. In some experiments, the subjects breathe through an apparatus that allows Kenney’s team to measure cardiac output at the same time they measure skin blood flow.
The researchers most often make that measurement on the inner surface of the forearm. They place on the skin a small donut-shaped device that can heat or cool just the dime-sized area inside the ring. Kenney can then use one of the laser techniques to measure the blood flood in that area. He can also infuse small amounts of a test substance just under the skin, to see how the substance affects flow and determine what molecules are involved in the process. Volunteers can have up to six rings set up on their arm at one time. That allows Kenney to compare blood flow under different treatments in the same part of the body, at the same time, in the same volunteer. “That’s important, because if we compare my blood flow to yours, we don’t know if a difference we see is because of the drug or just inherent variability in the way you and I respond,” he says. “In our experiments, everybody serves as their own control.”
Some experiments take place in two environmental chambers in Noll Laboratory that were specially built to study responses to environmental conditions. Each room has two layers of walls, one a couple of inches inside the other. Air that has been heated or cooled, humidified or dried, flows down from pores in the ceiling and back up through the space between the side walls, keeping the room at a constant temperature and humidity, with no hot or cold spots. Kenney can even add sun-mimicking lamps or make it “rain” inside the rooms.
“The range of temperature in here goes from about 40 degrees Fahrenheit to about 165 degrees Fahrenheit,” he says. “We can also change the humidity from very dry to very humid, so we can simulate an Arizona day or a Florida day.”
In other experiments, volunteers wear a water-perfused suit, a Lycra outfit that resembles scuba wear. It’s the same kind of suit worn by astronauts and fighter pilots to help them stay at a comfortable and safe temperature. Sewn into the suit is a network of narrow tubing. During an experiment, cold or warm water is pumped through the tubing to lower or raise the volunteer’s body temperature. A zippered flap in the suit gives researchers access to the skin on the forearm so they can measure blood flow under various conditions.
What stops working
Through dozens of series of experiments, Kenney, faculty collaborator Lacy Alexander, and their postdocs and students have explored why, as we age, the small vessels in our skin dilate less when we’re heated up and constrict less when we’re cooled. What, exactly, changes in older skin—and is there anything we can do about it?
“With aging, multiple changes occur in the skin, and they’re all conspiring against the ability to dilate and constrict skin blood vessels.”
They’ve found that one key is the small molecule nitric oxide (NO). Made in cells that line the blood vessels, NO plays a big role in vascular health in general.
“If there’s a lot of nitric oxide present, the vessels are healthy and they’re able to dilate appropriately,” says Kenney. “If you don’t have as much nitric oxide, the vessels are more constricted. That’s what happens in hypertension, that’s what happens with high cholesterol in some cases, and that’s what happens in aging.”
His group has traced the chemical pathways involved in nitric oxide production and found that at several steps, age-related changes limit the amount of NO we produce.
“With aging, multiple redundant changes occur in the skin, and they’re all conspiring against the ability to dilate and constrict skin blood vessels,” he says.
One of the most critical changes is a loss of BH4 (tetrahydrobiopterin), a cofactor necessary for the production of nitric oxide. Infusing BH4 directly into a small area of aged skin makes the vessels in that area respond like those of a 20-year-old, and taking BH4 in a pill enhances skin blood flow all over the body. Unfortunately, Kenney says, BH4 is made by only one company in the world and is very expensive—the yearly cost for one person would run into hundreds of thousands of dollars.
But he and former graduate student (now postdoctoral researcher) Anna Stanhewicz, who did the BH4 studies, realized that BH4 is chemically related to one of the B vitamins.
“There’s kind of a back-door way for the body to create BH4, and that is by taking folic acid in our diet,” says Kenney. Folic acid, also known as vitamin B9, can have serious side-effects when taken in too-large amounts, but it’s readily available, and it’s cheap. “We’re talking about pennies,” says Kenney “So we’re closer to identifying affordable intervention strategies.”
Deeper implications
Age-related changes in the nitric oxide pathway and other control mechanisms also limit the ability of vessels in our skin to constrict, which in turn makes us less able to stay warm in cold weather. As we get older, winters feel colder. Fortunately, we have easy ways to compensate: Turn up the heat, put on warmer clothing, drink hot tea or cocoa.
Even if cold snaps make us more uncomfortable as we age, they are not as likely to kill us as heat waves are. Kenney says the ability of older people to cope with high temperatures will become even more important in coming years because of increasing numbers of elderly people—“over 80” is the fastest-growing demographic group in the world—and the rising temperatures associated with climate change.
“The effect on human health isn’t so much that the average temperature on Earth is going up by a degree or a fraction of a degree every decade or so,” says Kenney. “The real danger is that when the average temperature shifts, so do the extremes. An increase in global temperature is associated with more frequent heat waves and more severe heat waves, and there’s a lot of evidence showing that that’s happening.”
Almost every summer in the past decade has brought at least one exceptionally deadly heat wave somewhere in the world. One of the worst hit Europe in 2003, during the hottest summer recorded in more than 400 years. Health officials reported that it caused 70,000 deaths, nearly 15,000 in Paris alone. Again, most of the victims were elderly.
“The changes we see in the skin precede and mimic things that happen with cardiovascular disease.”
Kenney’s work on thermoregulation has led him so deep into the details of how fine vessels dilate and contract that its significance now reaches beyond people’s ability survive a heat wave.
“It really plays into vascular health in general,” says Kenney. “We’re now using the skin circulation as a model for studying what’s going to happen to the coronary arteries, what’s going to happen to the carotids, what’s going to happen to those bigger, more important vessels later on in life—because the changes we see in the skin precede and mimic things that happen with cardiovascular disease.”
W. Larry Kenney is holder of the Noll Chair in Human Performance and Professor of physiology and kinesiology.