Adoptive cell-therapies, in which a patient’s own immune cells are used to recognize and target tumors, have shown breakthrough results for patients with certain B-cell malignancies, or cancers of the blood, but this therapy has not seen similar success in patients with solid tumors. Researchers at Baylor College of Medicine and Texas Children’s Cancer Center are working to change that, and a new study has shown promising results for several pediatric and adult solid tumor cancers.
In the study, published online in the journal Human Gene Therapy, researchers systematically evaluated a series of specially designed tumor-targeting molecules called chimeric antigen receptors (CARs) to determine which achieved the greatest anti-tumor activity when genetically engineered into special white blood cells called T cells.
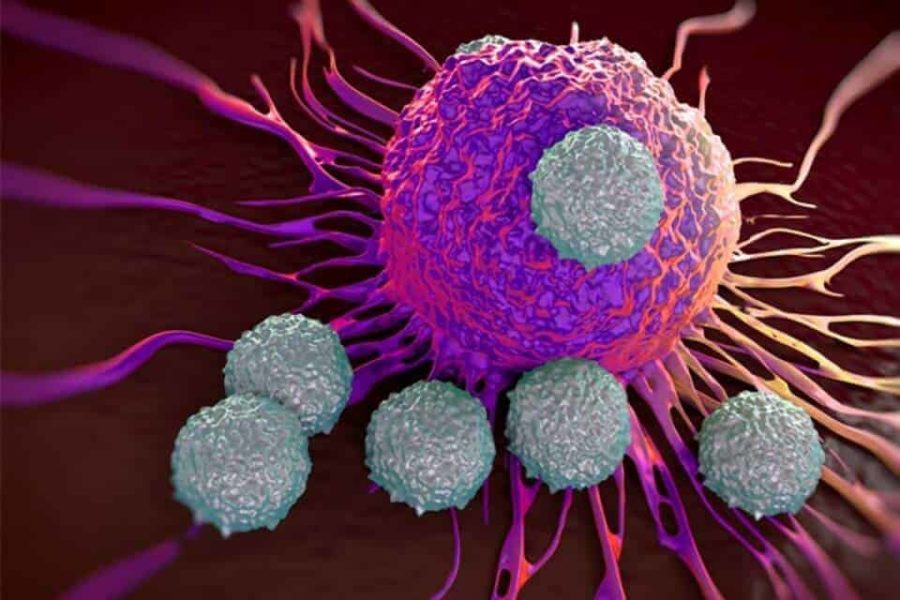
T cells – a type of unique immune cells involved in defense against tumors and infections – that have been programmed in the laboratory to express the tested CARs can recognize and attack tumor cells carrying one specific antigen on the surface of cancer cells.
“We set out an ambitious goal to develop and optimize chimeric antigen receptors that can target several solid tumors and will ultimately be studied in patients in a Phase 1 clinical trial,” said Dr. Andras Heczey, associate professor of pediatrics at Baylor and Texas Children’s Cancer Center, senior author of the study.
The engineered CAR T cells in this study targeted the molecule glypican-3 (GPC3), which is expressed on several solid tumors. Researchers compared several versions of GPC3-specific CARs that included distinct signaling endodomain combinations. Endodomains, the functional end of cell receptors where signals are transmitted, are important for expansion, survival and persistence of lymphocytes (white blood cells in the immune system, including T cells).
The research examined how these CAR T cells functioned in preclinical models of several solid tumors, including hepatocellular carcinoma and hepatoblastoma, which are both liver tumors, and malignant rhabdoid tumor, an aggressive cancer most commonly originating from the kidney.
Researchers found that the CAR containing the 41BB endodomain endows T cells with superior proliferative potential and potent antitumor activity, justifying further clinical development of this CAR for development as an immunotherapy for GPC3-positive solid tumors, said Heczey, who also is part of the Center for Cell and Gene Therapy at Baylor and Texas Children’s Hospital.
Heczey emphasized that systematic testing and optimization of chimeric antigen receptors is necessary for effective treatments against solid tumors. The next step for researchers is to test their optimized glypican-3-specific CAR in adults and children with glypican-3 expressing solid tumors.
“The approach we are developing is highly significant as we can now target several adult and pediatric solid malignancies, including hepatocellular carcinoma, hepatoblastoma, yolk sac tumor, malignant rhabdoid tumor and Wilm’s tumor.”
Others who contributed to this research include Wenpeng Li, Linjie Guo, Ekaterina Marinova, Xiuhua Gao, Stephen Gottschalk and Leonid Metelitsa of Baylor, the Center for Cell and Gene Therapy and Texas Children’s Cancer Center; Meng-Feng Wu and Hao Liu of Baylor’s Dan L Duncan Comprehensive Cancer Center; and Gianpietro Dotti of the University of North Carolina – Chapel Hill.
This work was supported by NIH/NCI grants (K12 CA090433 to AH; RO1 CA116548 to LM) Pablove Foundation Research Award and the Pediatric Pilot Award of Baylor College of Medicine.