Muscular dystrophy is a group of rare genetic diseases that cause progressive muscle weakness and deterioration. For decades, researchers have struggled to understand how the disease works and to find suitable treatments.
One of the major challenges is finding a good system in which to model the disease. Animals such as mice, often used to model human diseases, are not good analogues for muscular dystrophy in humans.
Now, researchers at the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) and the Wyss Institute of Biologically Inspired Engineering at Harvard University have developed a muscle-on-a-chip platform to study the disease. The platform led the researchers to a deeper understanding of how muscular dystrophy affects muscle formation and strength.
The research is published in The Journal of Cell Biology.
“In an era of advanced studies in rare diseases, patient analogs are going to be important,” said Kit Parker, Tarr Family Professor of Bioengineering and Applied Physics at SEAS and senior author of the paper. “In some rare diseases, there simply aren’t enough patients to run clinical trials. Organs on chips offer one such solution to this problem.”
Parker is also a Core Member of the Wyss Institute for Biologically Inspired Engineering at Harvard University.
“The drug discovery process for this disease has been going on for decades and this disease still lacks effective therapy,” said Peyton Nesmith, a graduate student at SEAS and first author of the paper. “Our goal was to develop, for the first time, a human form of this disease that could be studied to find new drugs, new treatments and to generally better understand the disease process in humans.”
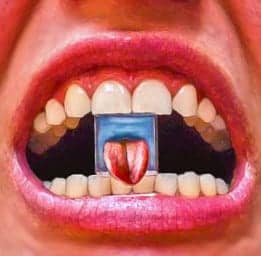
The team was inspired by a clinical test that uses tongue strength — how much pressure tongue bending generates against the roof of the mouth — to track the progression of the muscular dystrophy in patients.
“Clinically, it’s hard to compare muscle strength between patients because strength is dependent on so many things including what we eat, how much sleep we get, differences between men and women, and so on,” said Nesmith. “But clinicians figured out that we all use our tongues about the same. We wanted our experiment to make sense to a physician or clinician in that context.”
The team built the tongue-on-a-chip using stem cells from patients with Duchenne muscular dystrophy, a particular form of the disease. The researchers differentiated the stem cells to build skeletal muscle and used electrical stimulation to get them to contract like a bending tongue.
“The real benefit of this tongue on a chip assay is that it directly maps to a clinical diagnostic,” said Parker. “That is highly unusual in the organ on chips field. This work a physician anywhere in the world treating patients with Duchenne Muscular Dystrophy can look at this data and relate it directly to their own patients. For pharmaceutical companies, this is an extraordinary opportunity to start exploring medicinal therapeutics and gene editing therapies for these patients.”
Stem cells build muscle by aligning with one anther and fusing to form a muscle fiber. Healthy cells do this automatically with the proper cues. Previous research found that less mature stem cells, called satellite cells, from patients with Duchenne muscular dystrophy don’t follow these cues well but it was unclear whether more mature stem cells had the same problem.
The Harvard researchers found more mature stem cells, called myoblasts, are also implicated in Duchenne muscular dystrophy. These cells reacted slowly to cues, and did not fuse together as well, resulting in smaller, weaker muscles.
“This opens up a whole new avenue of research, exploring how can we direct these stem cells to behave like healthy ones and how drugs can signal these cells to promote healthy muscle formation to treat patients,” said Nesmith.
This paper was coauthored by Matthew A. Wagner, Francesco S. Pasqualini, Blakely B. O’Connor, Mark J. Pincus and Paul R. August. The research was supported by Sanofi-Aventis.