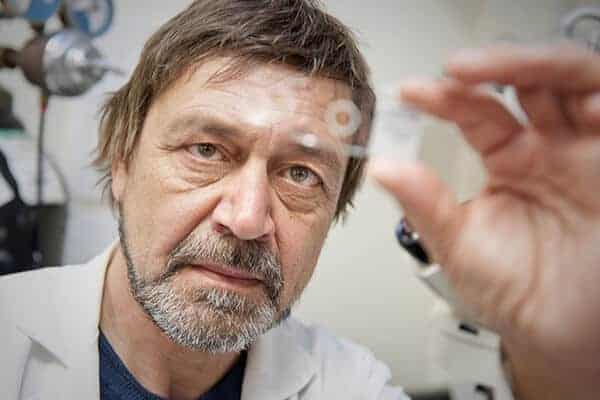
The marriage of two innovative technologies—one developed by Northeastern’s Slava Epstein, the other by the Broad Institute’s Paul Blainey—could accelerate both the discovery of new antibiotics that kill pathogens without encountering resistance and the diagnosis of specific pathogens causing disease, enabling fast, targeted treatments.
The new system, described in a paper in the journal Nature Communications, speaks to the Obama administration’s recent release of a National Action Plan to Combat Antibiotic Resistant Bacteria that calls for nationwide tracking of antibiotic resistance in pathogens using DNA sequencing.
Why DNA sequencing? Because it reveals a pathogen’s every move, whether offensive or defensive.
Four chemical compounds, called “bases,” make up the DNA of organisms from bacteria to us. The order, or sequence, of those bases determines the organism’s genetic inheritance. Taken together, the ordered bases—the “genome”—spell out the instructions for making and maintaining the entire organism. In the case of a bacterium, a particular sequence might code for a natural compound that kills other bacteria or, conversely, one that ensures its survival in the face of an attack from others. The killer compound could be a candidate for a new antibiotic, the protector compound the source of a bacterium’s antibiotic resistance, letting clinicians know which drugs not to prescribe if it hits.
The research team’s new lab-on-a-chip permits the screening of not only many more pathogens in record time at lower cost but also multitudes of pathogens that until now have not been available for analysis.
“The platform addresses the bottleneck in the overall sequencing of the genome, that is, the preparation of the DNA itself,” says Epstein, Distinguished Professor of Biology. “In the past, researchers had to grow massive amounts of bacteria and extract, purify, fragment, tag, and sort massive amounts of DNA from them, a costly and time-consuming process. This new system reduces the amount of DNA required 100-fold. We can use a tiny amount of cells—even 10,000 is enough—and produce superior sequencing analyses.”
A meeting of minds
Blainey’s lab at the Broad Institute of the Massachusetts Institute of Technology and Harvard developed the fundamental technology: a tool that automates the steps necessary to prepare the DNA for sequencing using just minuscule amounts of each liquid sample. It employs the science of “microfluidics”—the flow of liquids, usually in the range of microliters (one-millionth of a liter) to picoliters (one-trillionth of a liter), through micrometer-size channels.
Epstein’s iChip device expands the reach of Blainey’s technology immeasurably. The iChip isolates and grows small colonies of individual bacterial cells in their natural soil environment, permitting researchers to access the 99 percent of soil-based microorganisms that won’t grow in a lab, the so-called microbial dark matter.
In the past, researchers discovered new antibiotics by screening soil teeming with bacteria in the lab to find which ones produced compounds lethal to other bacteria. But today many bacteria, such as Staphylococcus aureus, have acquired mutations that render them resistant to current antibiotics. With the well of culturable bacteria essentially run dry, Kim Lewis, University Distinguished Professor of Biology, and Epstein cofounded the Cambridge-based biotechnology company Novobiotic Pharmaceuticals to plumb the microbial dark matter, with iChip in hand. There, they and their colleagues discovered teixobactin, a new antibiotic that kills pathogens without encountering resistance. They are on the fast track to discover more.
“With this platform, we can do high-throughput screening of genomes of culturable and of previously unculturable bacteria,” says Epstein. The paper describes success at sequencing both types accurately and quickly: The known pathogens Mycobacterium tuberculosis, whose slow growth stalls its diagnosis, and Pseudomonas aeruginosa, and new soil microcolonies produced via the iChip.
The findings address a critical concern of the recent Report to the President on Combating Antibiotic Resistance, which notes: “CDC has a large repository of well-characterized bacterial pathogens, but few have been sequenced to date.”
They also directly address patients’ needs. Given the very small samples the system requires, individuals could benefit from rapid by-the-bedside testing to diagnose the particular pathogens causing their disease as well as which antibiotics the sequenced pathogen might be resistant to.
“The high-throughput and high-accuracy sample preparation method presented here is positioned to power precision medicine, genomic surveillance, antibiotic-resistance tracking, and novel organism/natural product discovery on large scales,” the authors conclude.