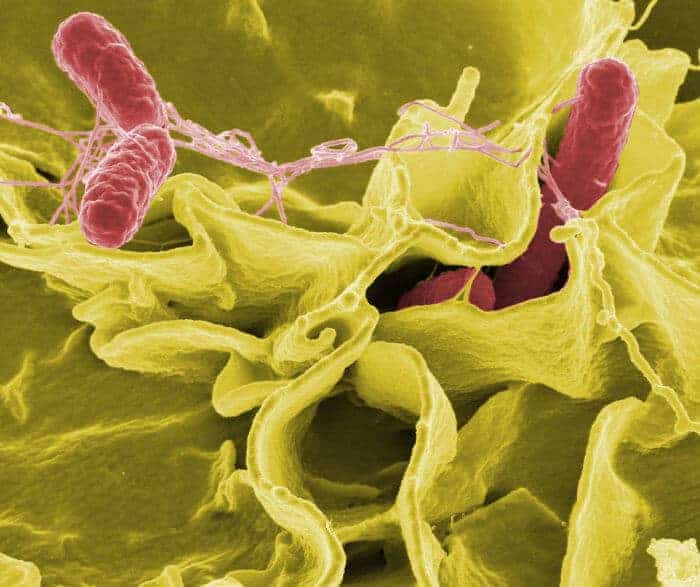
Typhoid fever, caused by a strain of the bacterial pathogen Salmonella, is thought to have wiped out one-third of the population of Athens in 430 B.C. and continues to afflict millions of people worldwide.
These days, the industrialized world’s familiarity with Salmonella comes about much more often through contact with one of its many non-typhoid-causing strains, in the form of severe food poisoning. There are as many as one million cases per year of Salmonella-caused food poisoning in the United States.
The Salmonella strains responsible for most food-poisoning cases occurring in developed countries pretty much limit their residence in the human body to the gut, where they secrete toxins that induce great gastrointestinal discomfort. But a mutant strain emerging in sub-Saharan Africa is uncharacteristically adept at breaking out of the intestine into the bloodstream, from which it can spread to other organs throughout the body and cause a lot of trouble.
A deadly combination of emerging multi-drug resistance on the bug’s part and poorly functioning immune systems on the part of the hungry children and HIV-infected adults who are most susceptible to infection makes this strain’s resulting rapid spread across continental Africa a matter of concern to public-health authorities.
Oddly, many patients infected with the mutant strain, which goes by the name ST313, lack classic gastrointestinal symptoms.
In a new study appearing in Cell Host & Microbe, Stanford bacteriologist Denise Monack, PhD, and her colleagues have figured out how ST313 manages to get out of the gut and perch elsewhere without getting pounced on and pounded to a pulp by the body’s immune system. In this Salmonella variant, a gene responsible for the production of a protein that’s highly immunogenic — in other words, it trips off a strong immune response — has been disabled, so the offending protein is no longer produced.
ST313’s resulting lack of this immunogenic protein (which must be good for something, but which the microorganism can apparently live without) is so non-immunogenic that the mutant marauder is able to hitch a ride inside a type of front-line immune cell whose job, ironically, is to sound the alarm when it encounters pathogens just like this one.
Once aboard its roving sentry-cell taxi, ST313 can travel undetected from the gut to the lymph nodes, spleen, and liver.
The same protein has been found to be inactivated in other mutant Salmonella strains that, like ST313, can escape the intestine (where nutrient resources are plentiful, but competition for them among trillions of individual microorganisms is fierce) and head for greener pastures in distant parts of the body. These so-called non-typhoidal Salmonella strains appear to be evolving toward becoming more like the typhoid-causing ones.
“By better understanding how Salmonella evolves to cause systemic disease in humans, we can better assess how dangerous emerging strains or outbreaks of Salmonella might be and mount the appropriate public health response,” Monack says.