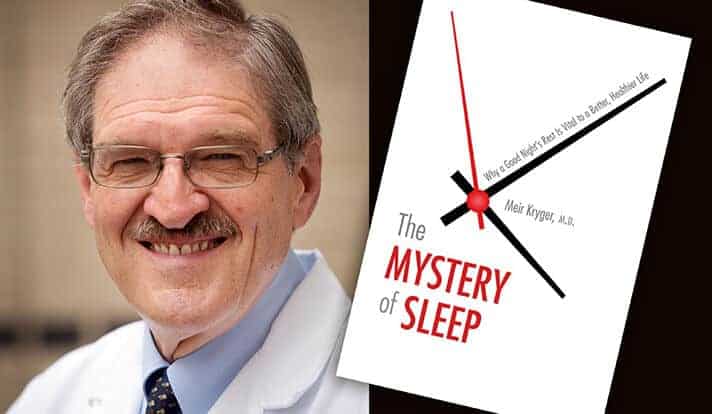
We spend one-third of our lives in bed, yet little is known about the purpose of sleep, says Dr. Meir Kryger, Yale professor of medicine and clinical professor of nursing. For more than 40 years, Kryger has been working to answer some of the remaining questions about sleep through innovative research and clinical practice. His latest book, “The Mystery of Sleep,” examines the many aspects of sleep and its disorders. Currently on sabbatical and participating in a popular sleep course at Stanford, Kryger is gathering information that he will bring back to a course for Yale students. YaleNews spoke to Kryger about his work, his latest book, and why getting a good night’s sleep matters. The interview has been edited.
What led you to focus on sleep as a specialty?
I became interested in sleep before there was a sleep specialty. When I was a medical resident at the Royal Victoria Hospital in Montreal, I had a patient, a gentleman who was having seizures while he was sleeping and was admitted to the hospital. I saw him one night struggling to breathe. I asked a friend of mine who was a neurosurgery resident to help set up equipment to study the patient while he was sleeping. We found that he stopped breathing, and his heart rate dropped while he slept — at times there were 10 seconds between breaths. That was the explanation for his seizures. His heart was actually stopping.
We treated the patient by doing a tracheoscopy, which is a hole in the windpipe. I decided to document the case and submit it for publication. At the time, there was almost nothing known about the clinical aspects of sleep. Zero. There was almost no research; there were a few papers done. I published that case and it was probably the first case of sleep apnea described in North America. It made me realize that this was a field that needed work, that needed researchers. That’s what got me interested and shaped most of the rest of my career. That was 1973.
“Not sleeping enough can result in impaired performance that can really harm people.”
The title of your book is “The Mystery of Sleep.” What remains a mystery to you?
We don’t really know the function of sleep. We know the many things that happen during sleep that appear to be good. There are hormonal changes that repair tissues. We think that memories are consolidated during sleep, especially during rapid eye movement (REM) sleep, which is dreaming sleep. But I’ll give you an example of what we don’t know: Newborn babies spend half their time in REM sleep. During this phase, REM, we know that we no longer control many of our bodily functions. For example, the heart rate becomes erratic, and breathing becomes erratic. We become like lizards in the sense that we no longer even control our temperature. We don’t understand this. We don’t understand whether a baby that spends half its time in REM is dreaming. And if so, of what? We have a zillion unanswered questions like that.
The book notes that there has been an upsurge of interest in sleep medicine in recent years. Why is that?
When I first started in the field, it was thought you close eyes, you go to sleep, you wake up, and everything is wonderful. There are many important things we’ve learned. For one, there are conditions during sleep that can be dangerous, and have the potential to worsen or cause other conditions. Number two, there’s been a huge amount of interest in the fact that not sleeping enough, or disrupted sleep, can result in impaired performance that can really harm people, and not just the person who is not sleeping enough, but the public. For example, there have been train accidents caused by locomotive engineers with sleep apnea, who fell sleep at the throttle. There are several other significant examples where sleepiness played a role: The Space Shuttle Challenger disaster, the Exxon Valdez oil spill, the Chernobyl Nuclear Plant explosion, and others. Not sleeping enough, having abnormal sleep, can result in significant danger to the public.
Your book details how sleep apnea was almost unheard of until the 1970s. How common is it and what do readers need to know about it?
It was so rare that there were publications that said it didn’t happen in women. We now know that it probably occurs in between 2% and 5% of adult women, which makes it almost as common as asthma. Right now, in America, it’s safe to say that at least 5% of men, and 2-4% of women have sleep apnea. What has happened since the 1970s is we’ve had an epidemic of obesity, and obesity is an important risk factor for sleep apnea. The average doctor now needs to know about sleep apnea because a large percentage of his or her patients will have it.
“The nightmares of posttraumatic stress disorder is a problem that still haunts the medical profession.”
What about the average person who can be at risk for sleep apnea, or have it and not know it. What do they need to know?
The most common symptom that we see in patients with sleep apnea is daytime sleepiness — falling asleep at the wrong time and place. That is by far the most common symptom, and it’s actually quite dangerous. People will drive trucks, cars; they’ll have family in their vehicles; and they have the potential of falling sleep. The bed partners are going to notice that at night the person stops breathing, and snores loudly. What’s most disturbing to the bed partner isn’t the noise of the snoring, but the terror of the silence when the person stops breathing. That’s a very common presentation. Often, the patient is in the clinic not because of their symptoms, but because the bed partner has observed something that is frightening.
What sleep problems do you see most frequently, and has that changed over your career?
The most common disorder we see in our sleep clinic at Yale is sleep apnea. We now also see patients with insomnia, where people have trouble falling asleep and staying asleep. We see people with sleepiness caused by sleep deprivation due to lifestyle. We see people with psychiatric disorders that have sleepiness, or inability to sleep, as a side effect of their medications.
There’s a condition called REM sleep behavior disorder in which people react to what they’re dreaming and they can harm a bed partner. This is an interesting condition because normally when we are dreaming, we are paralyzed. In people with this disorder, the system that paralyzes you during dreaming doesn’t work properly, and they may physically react to what they are dreaming.
Another thing we now recognize is that sleep disorders and sleep deprivation are very common in school-aged kids because in many places school start times are irrational. Teens, whose body clocks may not make them sleepy until well after midnight are not designed to wake up at 6 a.m. to go to class at 7 or 8 in the morning.
Another disorder that we see mostly in veterans, but also in others, is the nightmares of posttraumatic stress disorder. Patients wake up from terrible nightmares that have replayed the trauma that they witnessed or participated in, and it can go for 30, 40, 50 years. At the VA, for example, it is very common. I’ve had patients in the last couple of years at the VA who have PTSD from the Korean war. We’re talking about a war from the 1950s and the symptom has continued. Earlier in my career, I saw people who had gone through the Second World War either as soldiers or as prisoners in concentration camps who 30 or 40 years later were still having recurrent nightmares of what they had gone through. That’s a problem that still haunts the medical profession.
What sleep advice do people most often fail to follow?
The number-one piece of advice people ignore is to make sleep a priority. If you don’t get enough sleep, you’re going to have a rotten day: You’re going to be irritable; you may be dangerous behind the wheel. You have to make sleep a priority, and that means getting your 7 to 9 hours on the average so you won’t be so sleepy and dysfunctional during the daytime.
“When you improve sleep, you’re improving many other aspects of life.”
You’re currently on sabbatical. What project are you working on now?
I’m working on several. I’m at Stanford and participating in a course here, called “Sleep and Dreams.” The person who started the course and still teaches it is Dr. William Dement. This course has been running for 47 years, and it’s by far the most popular course at Stanford. A lot of famous people have taken that course over the years. Last year, I did a course for undergraduates at Yale, called “Mystery of Sleep.” As far as I know, it was the first undergrad course on sleep that Yale ever had. It was a wonderful experience for me and for the students. I wanted to see what made this similar course at Stanford stand out. I’ve learned a lot just by guest-lecturing this course and interacting with students. I met varsity athletes and Olympic medalists who had to change sleep and training schedules to perform maximally. One of the important lessons I learned from the course is that what you need to teach students is not just the science but also how proper sleep will improve their lives, no matter where their futures take them.
The other project I’m working on is a book, which I’ve been dying to do, looking at how artists look at sleep, and what goes through their mind when they are creating an image, be it a painting or sculpture, of someone sleeping. I’m working on that right now.
The third thing I’m going to do is research looking at a new treatment for sleep apnea. It’s a device that doesn’t require surgery. Over the years, I have seen a number of treatments come and go that didn’t work. We need better treatment. If this turns out to be a better treatment, that’s fabulous, but we need to do research to make sure it works.
What is your sleep ritual?
For me, the most important ritual is not a ritual but a belief that I follow: making sleep a priority. I plan my life to make sure that I’m going to get 7-9 hours. That to me is the most important thing I do. In a social setting whenever people hear that I’m a doctor who treats sleep disorders, they will tell me about their sleep problems. I give them the same advice: make sleep a priority. If they have difficulty staying awake during the day or sleeping at night, they should not ignore the symptom. Some sleep disorders are associated with heart disease, high blood pressure, metabolic disorders, mood disorders, and cognitive impairment. When you improve sleep, you’re improving many other aspects of life.