Lung adenocarcinoma, an aggressive form of cancer that accounts for about 40 percent of U.S. lung cancer cases, is believed to arise from benign tumors known as adenomas.
MIT biologists have now identified a major switch that occurs as adenomas transition to adenocarcinomas in a mouse model of lung cancer. They’ve also discovered that blocking this switch prevents the tumors from becoming more aggressive. Drugs that interfere with this switch may thus be useful in treating early-stage lung cancers, the researchers say.
“Understanding the molecular pathways that get activated as a tumor transitions from a benign state to a malignant one has important implications for treatment. These findings also suggests methods to prevent or interfere with the onset of advanced disease,” says Tyler Jacks, director of MIT’s Koch Institute for Integrative Cancer Research and the study’s senior author.
The switch occurs when a small percentage of cells in the tumor begin acting like stem cells, allowing them to give rise to unlimited populations of new cancer cells.
“It seems that the stem cells are the engine of tumor growth. They’re endowed with very robust proliferative potential, and they give rise to other cancer cells and also to more stem-like cells,” says Tuomas Tammela, a postdoc at the Koch Institute and lead author of the paper, which appears in the May 10 online edition of Nature.
Tumor stem cells
In this study, the researchers focused on the role of a cell signaling pathway known as Wnt. This pathway is usually turned on only during embryonic development, but it is also active in small populations of adult stem cells that can regenerate specific tissues such as the lining of the intestine.
One of the Wnt pathway’s major roles is maintaining cells in a stem-cell-like state, so the MIT team suspected that Wnt might be involved in the rapid proliferation that occurs when early-stage tumors become adenocarcinomas.
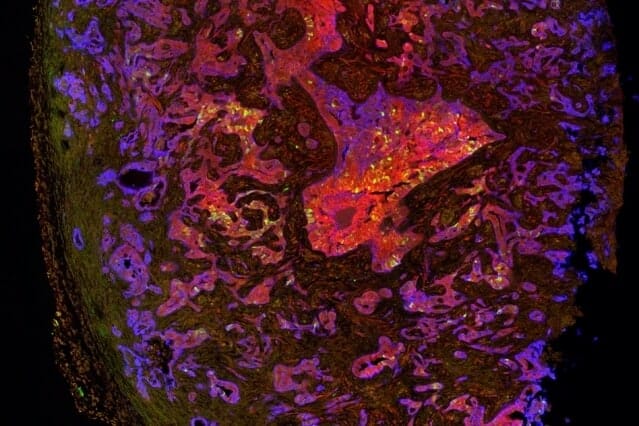
The researchers explored this question in mice that are genetically programmed to develop lung adenomas that usually progress to adenocarcinoma. In these mice, they found that Wnt signaling is not active in adenomas, but during the transition, about 5 to 10 percent of the tumor cells turn on the Wnt pathway. These cells then act as an endless pool of new cancer cells.
In addition, about 30 to 40 percent of the tumor cells begin to produce chemical signals that create a “niche,” a local environment that is necessary to maintain cells in a stem-cell-like state.
“If you take a stem cell out of that microenvironment, it rapidly loses its properties of stem-ness,” Tammela says. “You have one cell type that forms the niche, and then you have another cell type that’s receiving the niche cues and behaves like a stem cell.”
While Wnt has been found to drive tumor formation in some other cancers, including colon cancer, this study points to a new kind of role for it in lung cancer and possibly other cancers such as pancreatic cancer.
“What’s new about this finding is that the pathway is not a driver, but it modifies the characteristics of the cancer cells. It qualitatively changes the way cancer cells behave,” Tammela says.
Targeting Wnt
When the researchers gave the mice a drug that interferes with Wnt proteins, they found that the tumors stopped growing, and the mice lived 50 percent longer. Furthermore, when these treated tumor cells were implanted into another animal, they failed to generate new tumors.
The researchers also analyzed human lung adenocarcinoma samples and found that 70 percent of the tumors showed Wnt activation and 80 percent had niche cells that stimulate Wnt activity. These findings suggest it could be worthwhile to test Wnt inhibitors in early-stage lung cancer patients, the researchers say.
They are also working on ways to deliver Wnt inhibitors in a more targeted fashion, to avoid some of the side effects caused by the drugs. Another possible way to avoid side effects may be to develop more specific inhibitors that target only the Wnt proteins that are active in lung adenocarcinomas. The Wnt inhibitor that the researchers used in this study, which is now in clinical trials to treat other types of cancer, targets all 19 of the Wnt proteins.
The research was funded by the Janssen Pharmaceuticals Transcend Program, the Lung Cancer Research Foundation, the Howard Hughes Medical Institute, and the Cancer Center Support grant from the National Cancer Institute.