Women who have polycystic ovary syndrome (PCOS), a common hormone condition that contributes to infertility and metabolic problems, such as diabetes and heart disease, tend to have less diverse gut bacteria than women who do not have the condition, according to researchers at University of California San Diego School of Medicine, in collaboration with colleagues at Poznan University of Medical Sciences in Poland and San Diego State University.
The study is published online in The Journal of Clinical Endocrinology & Metabolism .
“The findings indicate women with PCOS tend to have less diverse populations of gut bacteria, a trend which appears to be linked to elevated testosterone levels,” said Varykina Thackray, PhD, senior author of the study and associate professor in the Department of Reproductive Medicine at UC San Diego School of Medicine.
The researchers examined fecal swabs from 73 women diagnosed with PCOS. Their samples were compared to swabs from 48 women who did not have PCOS and 42 women who had polycystic ovaries but did not have the other features of PCOS.
The study found the women who had PCOS had the least diverse gut bacteria, women who did not have the condition had the most diverse gut bacteria and women who had polycystic ovaries tended to have more diverse gut bacteria than women with PCOS, but less diversity than women without the condition.
“Our study suggests testosterone and other androgen hormones may help shape the gut microbiome, and these changes may influence the development of PCOS and the impact it has on a women’s quality of life,” said Thackray.
PCOS affects an estimated 7 to 10 percent of women of childbearing age, according to the Hormone Health Network. Women are diagnosed with PCOS when they have at least two of the three key features of the condition:
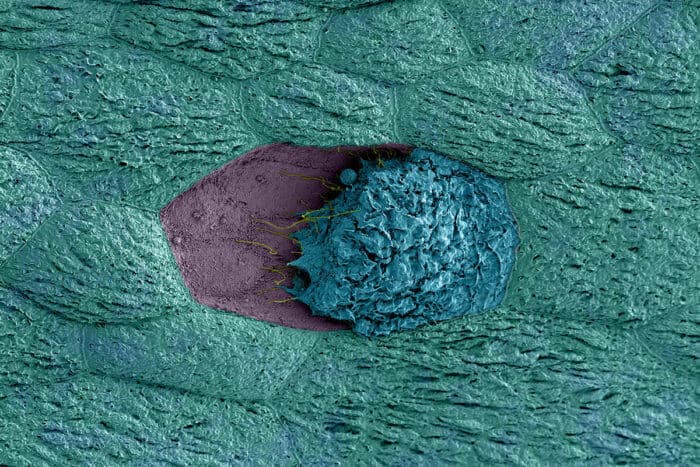
- Increased numbers of cysts in the ovaries (called polycystic ovaries) detected by ultrasound
- Slightly higher levels of testosterone or clinical symptoms, such as excess body hair
- Irregular or no menstrual periods
The diverse bacteria in the gastrointestinal tract play an important role in human health. Recent research suggests that gut bacteria differ in individuals with metabolic conditions, such as obesity, compared to individuals who do not have those conditions.
Thackray says additional research is needed to determine whether specific gut bacterial species contribute to the development of PCOS and whether the microbiome offers potential pathways for treating the condition.
“If testosterone drives the microbial composition of the gut, a compelling next step would be to determine if treatment of PCOS with testosterone blockers or oral contraceptives results in the recovery of the gut microbiome,” said Thackray. “It would also be important to figure out whether the gut microbiome of women diagnosed with PCOS using the criteria of polycystic ovaries and irregular or no menstrual periods is distinct from the gut microbiome of women diagnosed with the other subtypes of PCOS that require elevated testosterone.”
Co-authors of the study include: Antoni J. Duleba, University of California San Diego School of Medicine; Martyna Siakowska, Beata Banaszewska and Leszek Pawelczyk, Poznan University of Medical Sciences; Pedro J. Torres, and Scott T. Kelley, San Diego State University.
The research was supported, in part, by the National Institutes of Health’s National Institute of Child Health and Human Development (HD012303).
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!