In animal experiments, a human-derived glioblastoma significantly regressed when treated with the combination of an experimental enzyme inhibitor and the standard glioblastoma chemotherapy drug, temozolomide.
The regression seen in this combination therapy of temozolomide and the inhibitor SLC-0111 — which targets the enzyme carbonic anhydrase 9, or CA9 — was greater than that seen with either SLC-0111 or temozolomide alone, says research leader Anita Hjelmeland, Ph.D., assistant professor in the Department of Cell, Developmental and Integrative Biology at the University of Alabama at Birmingham.
“Our experiments strongly suggest that a strategy to target a carbonic anhydrase that is increased in glioblastoma, CA9, will improve temozolomide efficacy,” Hjelmeland said. “We believe the drug combination could improve patient outcomes in glioblastomas sensitive to chemotherapy.”
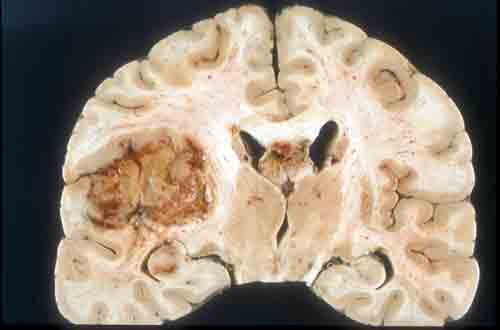
Glioblastoma is the most common primary brain tumor seen in adults. Half of the tumors recur less than seven months after undergoing the standard treatment of surgery, temozolomide and radiation. The median survival after diagnosis of this deadly cancer is 12 to 14 months. Thus, new approaches to therapy are urgently needed.
Solid tumors like glioblastoma create microenvironments within and around themselves. A common condition is hypoxia, a shortage of oxygen as the tumor outgrows its blood supply. Tumor cells shift to making their energy through glycolysis, a method of metabolism that does not require oxygen. Glycolysis, in turn, changes the acid-base balance at the tumor — the extracellular space becomes more acidic and the tumor cell interiors become more alkaline, adapting to this change.
In the face of this hypoxia and acid stress, tumor cells over-produce CA9, a membrane enzyme that converts carbon dioxide and water to bicarbonate and protons. This reaction aids maintenance of the altered acid-base balance in the tumor microenvironment.
Thus, CA9 is a possible therapeutic target, and the inhibitor SLC-0111 shows more than 100-fold specificity against CA9, versus two other forms of human carbonic anhydrases, CA1 or CA2. Furthermore, collaborators on this project have previously shown that SLC-0111 exhibits effectiveness against breast cancer xenografts in animals. SLC-0111 has been tested in Phase I clinical safety trials sponsored by Welichem Biotech Inc. in Canada for patients with advanced solid tumors.
The research team led by Hjelmeland and co-first authors Nathaniel Boyd, Ph.D., and Kiera Walker, both working in Hjelmeland’s UAB lab, studied glioma cells in cell-culture that were derived from an aggressive pediatric primary glioblastoma and from an adult recurrent tumor. The researchers also studied the tumor in mice, using the adult recurrent glioblastoma.
One reason for recurrence of glioblastoma is a therapeutically resistant sub-population of glioma cells known as brain tumor initiating cells. Part of the focus of the Hjelmeland team was to look at the effect of the combination therapy on that subset of glioblastoma cells.
The researchers found that the combined treatment with temozolomide and SLC-0111 in cell culture experiments: 1) reduced glioblastoma cell growth, 2) induced arrest of the cell-division cell cycle by creating breaks in DNA, 3) shifted the tumor metabolism and intracellular acid-base balance by decreasing metabolic intermediates, and 4) inhibited enrichment of brain tumor initiating cells.
In experiments with mice, the combined treatment with temozolomide and SLC-0111: 1) delayed tumor growth of a patient-derived, recurrent glioblastoma xenograft implanted beneath the skin of immunocompromised mice, as compared to temozolomide alone, and 2) improved survival of the mice when the xenograft was implanted in the brain, a placement that more closely models glioblastoma in patients.
“Clinical trials in glioblastoma often initiate with patients that have a tumor recurrence, and we have demonstrated in vivo efficacy for SLC-0111 with temozolomide in a recurrent glioblastoma,” the researchers wrote in their study, published in JCI Insight. “Therefore, our data strongly suggest the translational potential of SLC-0111 for glioblastoma therapy.”
“With funds from the Southeastern Brain Tumor Foundation,” Hjelmeland said, “we continue to determine whether there are subtypes of glioblastomas that are most likely to respond to combinatorial therapy.”
Co-authors with Hjelmeland, Boyd and Walker in the paper, “Addition of carbonic anhydrase 9 inhibitor SLC-0111 to temozolomide treatment delays glioblastoma growth in vivo,” are Joshua Fried and Bo Xu, M.D., Ph.D., Southern Research, Birmingham, Alabama; James R. Hackney, M.D., UAB Department of Pathology; Paul C. McDonald, Ph.D., and Shoukat Dedhar, Ph.D., BC Cancer Research Centre, Vancouver, British Columbia, Canada; Gloria A. Benavides, Ph.D., and Victor Darley-Usmar, Ph.D., UAB Center for Free Radical Biology; Raffaella Spina, Ph.D., and Eli E. Bar, Ph.D., Case Western Reserve University, Cleveland; Alessandra Audia, Ph.D., and Krishna P. Bhat, Ph.D., MD Anderson Cancer Center, Houston; Sarah E. Scott, Catherine J. Libby, Anh Nhat Tran and Mark O. Bevensee, Ph.D., UAB Department of Cell, Developmental and Integrative Biology; Corinne Griguer, Ph.D., and G. Yancey Gillespie, Ph.D., UAB Department of Neurosurgery; Susan Nozell, Ph.D., UAB Department of Radiation Oncology; Burt Nabors, M.D., UAB Department of Neurology; and Emily Gordon, Ph.D., and Sara J. Cooper, Ph.D., HudsonAlpha Institute for Biotechnology, Huntsville, Alabama.
This work was supported by National Institutes of Health grant CA200085, NS096531, CA1515122, the UAB Brain Tumor SPORE CA151129 Career Development Award, a pilot award from the UAB-HudsonAlpha Center for Genomic Medicine, and startup funds from UAB.
Additional support was provided by NIH grants NS100054, CA160821, CA138517, RR027822-01, NS47466 and AI027767.
Hjelmeland, Gillespie, Nabors, Darley-Usmar, Griguer and Nozell are all members of the UAB Comprehensive Cancer Center, one of the nation’s leading cancer research and treatment centers.