Can whole genome sequencing illustrate changes in drug susceptibility of gonorrhoea to antimicrobials used for treatment and so help to define more effective treatment regimens? The first study of this kind within an international surveillance programme for sexually transmitted infections shows distribution of drug-resistant gonorrhoea strains across Europe. The study results are published in an ECDC report and summarised in The Lancet Infectious Diseases.
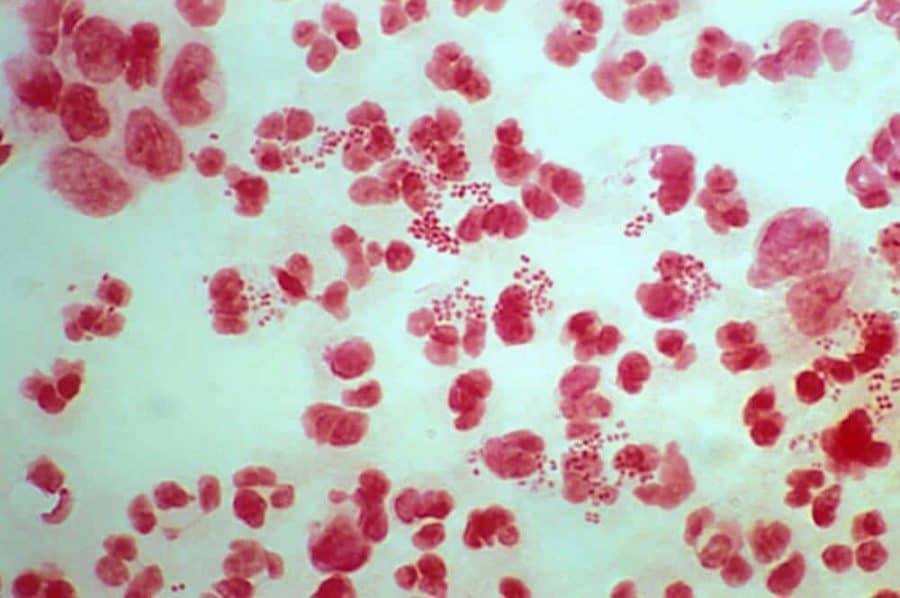
With more than 75 000 reported cases in 2016, gonorrhoea is the second most commonly notified bacterial sexually transmitted infection (STI) in Europe. But over the past decades, Neisseria gonorrhoeae, the bacterium causing gonorrhoea, has been developing resistance to several antimicrobial classes as shown by the European Gonococcal Antimicrobial Surveillance Programme (Euro-GASP). This programme is co-ordinated by ECDC and annually monitors emerging resistance trends by testing susceptibility of the recommended antimicrobial agents for gonorrhoea treatment.
Previous Euro-GASP results indicate that susceptibility to antimicrobials and resistance patterns have changed over the years in the European Union and European Economic Area (EU/EEA). Resistance to cefixime decreased since 2010 and while resistance to azithromycin dropped between 2010 and 2012, it subsequently increased again from 2013 onwards.
In the light of limited alternatives to the current recommended combination therapy with ceftriaxone and azithromycin (introduced in 2012), and recent reports of extensively drug resistant gonorrhoea strains, it is vital to understand if changes in resistance prevalence are the consequence of modifications in treatment, sexual behaviour in different sexual networks, the gonococcal strain distribution or due to other reasons.
ECDC expert Gianfranco Spiteri says: “Drug-resistant bacteria are becoming a huge public health threat. To control them, we badly need new tools to identify and track new infections and antibiotic resistant strains. The new approach we used in our study will allow European-wide genomic surveillance of gonorrhoea, which directly influences infection control on a national level and helps to prevent gonorrhoea. This approach can also be expanded to other infections”.
Clear public health benefit
In collaboration with the Centre for Genomic Pathogen Surveillance, the Wellcome Sanger Institute, Public Health England and the Örebro University Hospital, ECDC collected, typed and analysed more than 1 000 isolates from 20 countries to assess the public health relevance of whole genome sequencing (WGS) in the surveillance and control of Neisseria gonorrhoeae.
The study showed the clear public health benefit of WGS over traditional typing methods, particularly when linked with epidemiologic data, as it increases the understanding of the dissemination of strains and resistance within a population. Other advantages are increased precision and detail as well as predicting antimicrobial resistance relatively well. WGS thus facilitates the development of more targeted intervention strategies, especially if associations between molecular type and epidemiological characteristics are well defined. With this information widely available, WGS could support health professionals in identifying the most effective antibiotics for gonorrhoea treatment in their region.
As part of the study, ECDC and its partners also stored the WGS data in an openly accessible genomic database of gonorrhoea. This database allows real-time surveillance of gonorrhoea, which public health officials can use for monitoring of strains and possible changes of resistance patterns to the commonly used antibiotics.