People living with cystic fibrosis spend their lives battling chronic lung infections resistant to antibiotic therapy. A one-size-fits all approach to wiping out the bacterium may not be the best approach for all patients with the disease, according to a new study led by Pieter Dorrestein, a professor at the University of California San Diego, and Robert Quinn, a Michigan State University researcher who conducted the research at UC San Diego.
Researchers discovered that tweaking other factors in a cystic fibrosis lung model, such as pH balance and oxygen, helped eradicate pathogenic bacteria while minimizing risks of antibiotic resistance and overgrowth of other microorganisms.
“We think of antibiotics as causing a ‘scorched earth,’ simply wiping an unknown portion of both healthy and hopefully bad bacteria,” Dorrestein said. “We actually have a poor understanding of what happens to their microbiota when people take antibiotics — both healthy people and people with cystic fibrosis.”
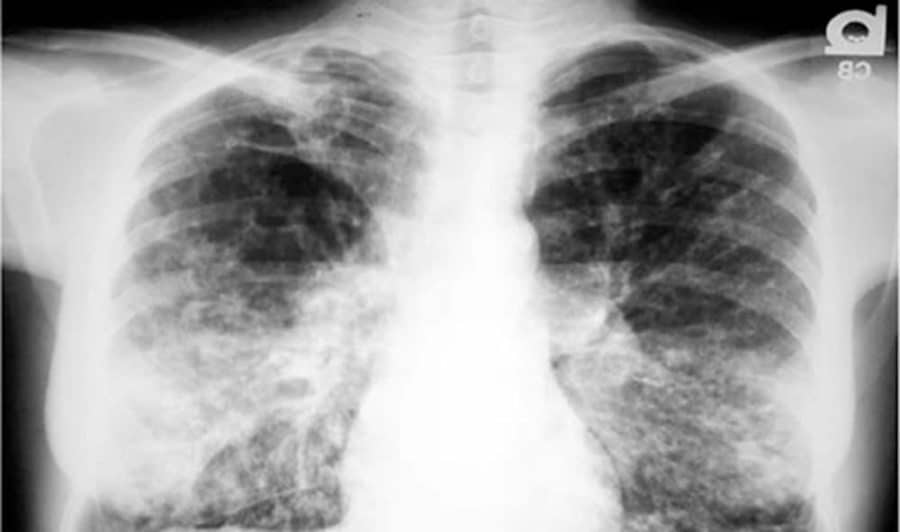
Due to the genetic defect that underpins cystic fibrosis, a thick, sticky mucus builds up in the lungs of patients. The mucus helps microorganisms to thrive. One problematic bacterium, Pseudomonas aeruginosa, also forms a biofilm in the lung, which is difficult for the immune system and antibiotics to penetrate. These lung infections are a serious and chronic problem for many people living with cystic fibrosis. Currently, the infections are largely managed by trial-and-error with a combination of antibiotics, antifungals and anti-inflammatory molecules.
Scientists typically study bacterial infections by analyzing one specific type of bacteria and its interactions with human cells. Quinn looks at the cystic fibrosis lung as a whole, living in a unique environment in which a particular bacterium doesn’t operate alone, but interacts with other microbes in the community, the human cells that make up the lung and other molecules, chemicals and metabolites. All of which behave like an ecosystem.
Quinn developed a system called WinCF, which provides pH and oxygen gradients that mimic the narrow tubes that make up human lung bronchioles.
Quinn and his team collected sputum samples from 18 patients with cystic fibrosis and applied them to the WinCF system in their lab. They altered factors such as pH, oxygen levels and antibiotics to map approximately 600 different cystic fibrosis lung conditions.
Researchers found that microbes in cystic fibrosis lungs divide themselves into two distinct communities: known pathogens, or microbes that can cause health problems, which live in high pH and oxygen-rich regions, and anaerobes, or microbes that thrive in areas with low pH and little oxygen.
“This stratification matters because it may affect treatments for cystic fibrosis patients,” Quinn said. “For example, certain bacteria may survive antibiotic treatment because they can hide deeper in the lung mucus. Meanwhile, the bacteria that are killed off may open up space for other microbes to grow, potentially creating a new set of problems.”
When they added the anti-Pseudomonas aeruginosa antibiotic, tobramycin, to the top culture in their WinCF model, researchers saw drastic changes in the system’s microbial makeup. Some bacterial species were killed in all regions of the column, some killed in the higher, more oxygen-rich layers, but survived at lower depths, while other species continued to thrive at the lower depth.
Quinn said he was surprised to see blooms of Aspergillus fungi spring up in the regions previously occupied by the killed bacteria. Aspergillosis, the infection caused by this fungus, is not uncommon in cystic fibrosis patients treated with antibiotics.
Not only did the antibiotic shift the microbial balance in the cystic fibrosis lung model, the chemical structure of the antibiotic itself was modified by the microbes. This alteration could help bacteria resist its effect.
“Antibiotics alter the overall structure and relationships in a dynamic community, and not always in a way that’s beneficial for the patient,” Quinn said. “We don’t yet know the ‘rules’ for tipping the balance in favor of a beneficial microbial balance.”
When the researchers lowered the pH of the cystic fibrosis mucus in the WinCF system by one unit, the bacterial makeup of the sample shifted from 70 percent to essentially none.
While the WinCF system should not be used to influence patient care just yet, Dorrestein said the ultimate goal is a “precision-care” clinic for patients with cystic fibrosis. In this scenario, physicians and technicians could rapidly analyze each patient’s sputum for unique molecular and microbial patterns and test different combinations of treatment options in the lab — pH change, oxygen levels, antibiotics — before prescribing them to the patient.
Additional study co-authors include: William Comstock, James T. Morton, Ricardo da Silva, Alda Tran, Alexander Aksenov, Louis-Felix Nothias, Alexey V. Melnik, Gail Ackermann, Douglas Conrad, Rob Knight, UC San Diego; Tianyu Zhang, Montana State University; Daniel Wangpraseurt, University of Cambridge and UC San Diego; and Isaac Klapper, Temple University.