Researchers have discovered how specific cells in the guts of mice slow down metabolism and eventually contribute to obesity, diabetes, hypertension and atherosclerosis. The findings, scientists say, could have important implications for the prevention and treatment of these kinds of metabolic diseases in humans. The study was funded by the National Heart, Lung, and Blood Institute (NHLBI), part of the National Institutes of Health and appears in the journal Nature.
“With this research we are connecting the dots between gut metabolic food sensors and cardiovascular disease; and might open new therapeutic avenues to treat patients with a host of related conditions,” said Michelle Olive, Ph.D., program officer at the NHLBI Division of Cardiovascular Sciences.
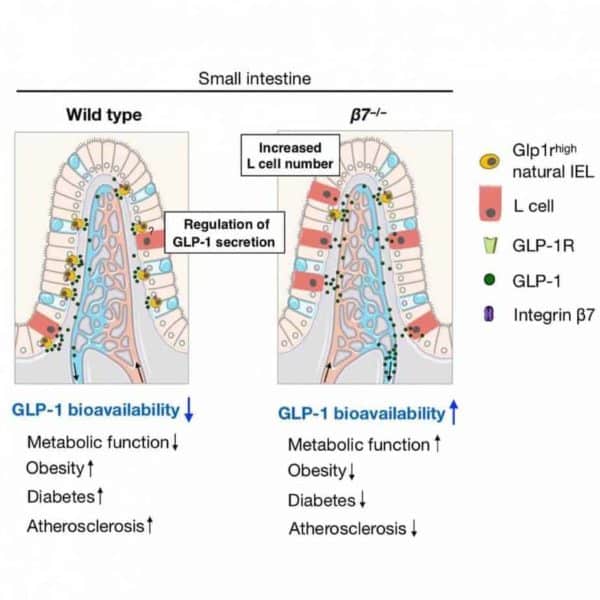
The cells are called intraepithelial T lymphocytes (or natural IELs), and when they are not present, researchers discovered, the metabolism of mice goes into overdrive.
“The mice become metabolically hyperactive and, even when consuming a diet very high in fat and sugar, are able to resist metabolic diseases such as obesity, hypertension, hypercholesterolemia, diabetes, and atherosclerosis,” said the study’s lead researcher Filip Swirski, Ph.D., an associate professor at Harvard Medical School and Massachusetts General Hospital, Boston.
When natural IELs are present, however, the researchers found that they limit the availability of a type of hormones, incretin GLP-1, that help speed up metabolism. By limiting GLP-1, the natural IELs, in effect, slow down the body’s metabolism and conserve the energy it gets from food.
Over millions of years of evolution, this efficient use of energy provided an essential advantage: when food was scarce, organisms stored rather than burn some of the ingested energy, and they survived longer.
“Now with food so abundant, this energy-saving mechanism can backfire and lead to unhealthy outcomes,” explained Swirski.
Swirski’s research could eventually shed light on how to prevent and treat cardiovascular disease and other related ailments in humans. The first step is to determine the number and variations of natural IELs in people, then answer key questions. Do individuals with low numbers of IELs get protected against cardiovascular disease? Could blocking IELs reduce their risks?
“Looking forward, we need to better understand IELs function in metabolism,” said Swirski. “We also need to know whether therapeutic targeting of IELs in humans can be a treatment for obesity, hypercholesterolemia, diabetes, and hypertension.”
This publication is supported by NHLBI grant R35HL135752.