The microbiome is a collection of trillions of bacteria that reside in and on our bodies. Each person’s microbiome is unique — just like a fingerprint — and researchers are finding more and more ways in which it impacts our health and daily lives. One example involves an apparent link between the brain and the bacteria in the gut. This brain-gut “axis” is believed to influence conditions such as Parkinson’s disease, depression, and irritable bowel syndrome. However, many studies into the brain-gut axis have stalled because of one central problem: the lack of an adequate testable model of the gut.
Current testing platforms cannot emulate the human gut accurately and cheaply enough for large-scale studies. The research community needs something new, which is what a team at MIT Lincoln Laboratory is tackling in a project funded through the Technology Office. Researchers there aim to create the perfect artificial gut.
“The question from the mechanical side is, how do you emulate the colon?” says Todd Thorsen, the project’s principal investigator from the Biological and Chemical Technologies Group. “Bacteria in the colon occupy lots of ecological niches.”
Thorsen is referring to the complexity of the human gut, which includes a community of 100 trillion microbes that all have specific, and sometimes clashing, needs. For example, certain types of bacteria in the gut will die in the presence of oxygen, while others need it to survive. The gut also contains both hard and soft mucus that allows different types of bacteria to grow. All of these conditions need to be mimicked in a single platform in order to properly maintain and test microbiome samples — and that’s not an easy task.
“Until now, no one has been able to culture a microbiome sample and maintain it,” says David Walsh from the Biological and Chemical Technologies Group, who led the device’s development and fabrication. “If we can maintain a culture, we can do things like add toxins and therapeutics to see how they change the culture over time.”
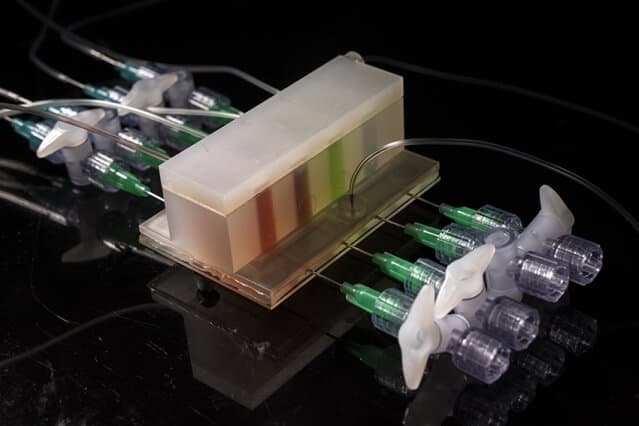
To address the problem, the laboratory team developed a multimaterial platform made of permeable silicon rubber and other plastics, such as polystyrene, all of which are cheap and can be rapidly prototyped. The two components of the platform emulate the essential oxygen and mucosal gradients.
The above photo (left) shows the component that controls the oxygen gradient. Air diffuses through the plastic while the blue ports allow researchers to change the local oxygen concentrations at different positions within the adjacent microculture chambers. The right photo shows the component that controls mucus, which is welled up into the device from below. Both components implement careful geometry to yield the precise conditions found in the gut.
“The final system will allow us to tackle real-world problems,” Walsh says. Those problems, in addition to unraveling the brain-gut axis, include developing resilience to current and emerging pathogens, combating biological warfare, and more.
This year, the research team is partnering with the University of Alabama at Birmingham, Northeastern University, and the University of California at San Francisco to implement their first tests of microbiome samples to study links to Parkinson’s disease. The laboratory’s role is to use the artificial gut to culture microbiome samples taken from people with and without Parkinson’s disease and test what happens when different suspected adverse influencers are added. The goal is to correlate how changes in the microbiome caused by exposure to certain toxins may induce Parkinson’s-like nerve damage.
The laboratory will also continue advancing other aspects of the project. Some examples include building a tubular core-shell origami-like gut that rolls up during assembly to emulate the colon and the surrounding vascularized tissue, and developing modeling software to predict how microbial communities might change over time.