The net clinical benefit of anticoagulants for atrial fibrillation (AF) – one of the most important causes of irregular heartbeats and a leading cause of stroke – decreases with age, as the risk of death from other factors diminishes their benefit in older patients, according to a study led by researchers at UC San Francisco.
The multi-institutional study of nearly 15,000 AF patients found that the anticoagulant warfarin was not beneficial after age 87 and another, apixaban, after age 92. As a result, physicians should consider all mortality risks, such as cancer and end-stage kidney disease, when recommending anticoagulants to older adults with AF, the researchers said.
The study is online Nov. 11, 2019, in Circulation: Cardiovascular Quality and Outcomes (CCQO), to coincide with a presentation at the annual American Heart Association Scientific Sessions 2019.
“Many prior studies looking at the benefit of blood thinners found older adults benefit more than younger adults, but they narrowly focus on atrial fibrillation and strokes and don’t account for all other health conditions affecting older adults,” said lead author Sachin Shah, MD, MPH, assistant professor of medicine at UCSF. “Our study is the first to find that when taking these factors into consideration, anticoagulant benefit actually decreases with age.”
Atrial fibrillation affects an estimated 2.2 million Americans, according to the National Stroke Association, and about 15 percent of people who have strokes have AF. The stroke association estimates that up to 80 percent of strokes among people with AF could have been prevented.
While patients age 75 and older are at higher risk for stroke and advised to use anticoagulants, there is little evidence of their net benefit in this population. Advancing age also increases the likelihood of death from non-AF causes, thereby limiting the benefit or harm from AF and anticoagulant treatment.
Indeed, anticoagulant use in older patients with atrial fibrillation is similar to prostate specific antigen (PSA) testing. PSA testing is common in elderly men, despite evidence that those without aggressive prostate cancer are unlikely to benefit from diagnosis and treatment and may face significant risks for quality of life if they undergo prostate surgery.
“Competing risk of death is an important consideration when estimating the net clinical benefit of anticoagulation therapy,” Shah said. “Failing to account for competing risks likely overestimates the net clinical benefit of anticoagulation, an effect that is more pronounced at older ages and with more effective anticoagulants.”
In the CCQO study, Shah and his colleagues, including collaborators from Kaiser Permanente Northern and Southern California, reviewed the records of 14,946 adults from January 2006 to June 2009 in the Anticoagulation and Risk Factors in Atrial Fibrillation-Cardiovascular Research Network. They selected patients age 75 and older, with an average age of 81.
The researchers used a computerized decision analytic model called the Atrial Fibrillation Decision Support Tool (AFDST), developed by the University of Cincinnati, to determine the potential benefit of anticoagulants. The model uses patient characteristics and guidelines on AF treatment from the American College of Cardiology, American Heart Association and Heart Rhythm Society to offer a recommendation.
The research team estimated the lifetime net clinical benefit of warfarin and apixaban relative to no treatment in quality-adjusted life years (QALY). QALY is a measure of disease burden that includes both the length of life and its quality, with one QALY equaling one year in perfect health.
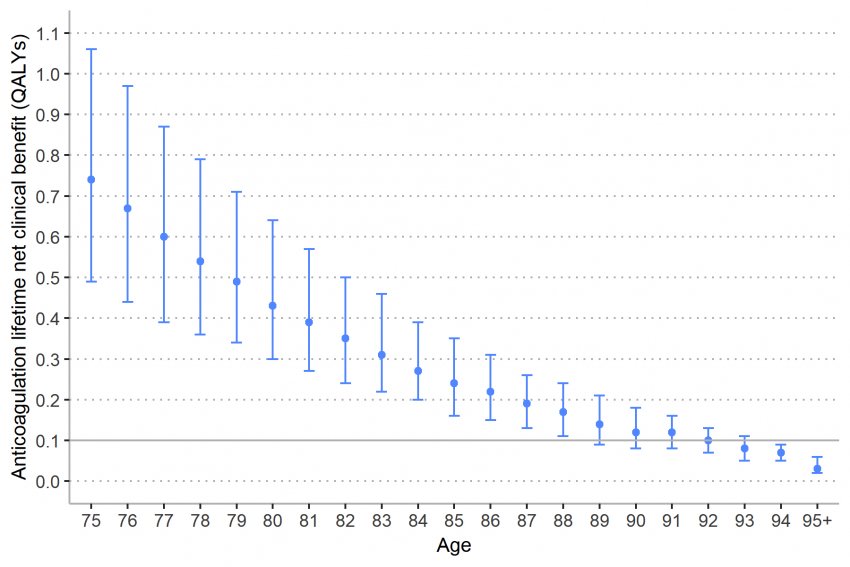
Using 0.10 lifetime QALYs as the minimal net clinical benefit, warfarin started at 0.45 QALYs at age 75, then fell below 0.10 at age 87, while apixaban started at 0.74 QALYs at age 75, then fell below 0.10 at age 92.
“For years, we have been telling our doctors and patients that we are not being aggressive enough in providing anticoagulant therapy to our patients with atrial fibrillation, and it’s a national problem,” said senior author Mark Eckman, MD, the Posey Professor of Clinical Medicine at the University of Cincinnati College of Medicine. “This study now adds a caution, acknowledging that while undertreatment is a major concern, at advanced years of age, maybe we should be a little more thoughtful and careful in our treatment decisions about anticoagulation.”
Co-Authors: Margaret Fang, of UCSF; Kristi Reynolds, of Kaiser Permanente Southern California; Alan S. Go, of Kaiser Permanente Northern California and UCSF; and Daniel Singer, of Massachusetts General Hospital and Harvard Medical School.
Funding: Funded by the National Institutes of Health (NIH) National Center for Advancing Translational Sciences (NCATS UL1TR000077-05); National Heart, Lung, Blood Institute (U19HL91179, 1RC2HL101589); and National Institutes on Aging (R01 AG15478). Shah was partly supported by the UCSF Division of Hospital Medicine, and Singer was partly supported by the Eliot B. and Edith C. Shoolman Fund of Massachusetts General Hospital.
Disclosures: Eckman has current or recent investigator-initiated grant funding from the Heart Rhythm Society through a grant from Boehinger-Ingelheim Pharmaceuticals, Inc., NCATS (UL1TR000077-05), NIH National Institute of Child Health and Human Development (R01HD094213), Virus Action Coalition of the Centers for Disease Control, Merck, Pfizer Educational Group, Bristol-Myers Squibb/Pfizer Education Consortium, and the Cystic Fibrosis Foundation. Go has a research grant through Kaiser Permanente Northern California Division of Research from iRhythm Technologies. Reynolds has received research support through Kaiser Permanente Southern California Department of Research & Evaluation from iRhythm Technologies. Singer receives research support from Bristol-Myers Squibb and Boehringer-Ingelheim and serves as a consultant or an advisory board member for Bristol-Myers Squibb, Boehringer-Ingelheim, CVS Health, Johnson and Johnson, Merck, and Pfizer.


