Radiation therapy to treat cancer can be grueling, requiring consecutive days of therapy over days or weeks.
“When you talk to patients about coming in for 35 treatments, or seven weeks of daily therapy, usually their face kind of sags in disappointment or perhaps apprehension,” says Keith Cengel, a radiation oncologist at Penn’s Perelman School of Medicine.
That’s why the promise of what’s known as FLASH radiation therapy, in which a full dose of radiation is given in less than a second, is so great.
But FLASH remains in its infancy, with researchers still unsure about how the all-in-one-go approach stacks up against traditional methods. To test its effectiveness at killing cancer cells and sparing normal cells, researchers from Penn Medicine and Penn’s School of Veterinary Medicine are pairing their expertise in a clinical trial applying the cutting edge of human medicine in dogs.
“From a veterinary standpoint, this is a type of radiation that is still very, very new in human medicine,” says Jennifer Huck, a veterinary surgeon at Penn Vet who is partnering with Cengel on the trial. “So there’s a lot of excitement in the veterinary realm about this.”
In the trial, dogs with osteosarcoma, a form of bone cancer that people, especially children, can also develop, receive the FLASH radiation. They then go on to receive the standard of care for osteosarcoma, which entails amputating the affected limb and, in some cases, at the owners’ and veterinarian’s discretion, following up with chemotherapy to slow the growth of microscopic disease in other areas of the body that may already be present at the time of diagnosis.
The study is not designed to confer a direct benefit to the dogs enrolled, though the clinicians aren’t ruling out that possibility. The main intent, they say, is to understand what’s happening to the cells and tissues—both cancerous and normal—that the therapy targets. In labs both at Penn Medicine and Penn Vet, researchers are studying samples from the amputated limb to assess the effects of the treatment.
“We’re looking at gene expression profiling, markers of cell death and cell division, and analyzing immune cell populations to just get a survey of what the tumor and normal tissue look like,” says Cengel.
The work is moving quickly. The project aims to enroll 20 dogs. The researchers started late in 2019 and have already treated seven. Several more await treatment or evaluation.
“I think that we greatly underestimate the excitement of pet owners to be involved in research and to be able to contribute to a project like this,” says Huck. “The treatment that their pet receives is ultimately no different from any other standard of care that we would offer to any pet that comes in with osteosarcoma, whether they’re on the study or not, so I think that also gives them comfort.”
Learning from Milo
Four-year-old Milo, a leggy Saint Bernard, is one such participant. Owner Tim Gordon describes him as “perfect.”
“He’s a great dog, great with the kids, great with our other dog,” Gordon says. “He’s adjusted to everything we’ve thrown at him.”
Starting around Thanksgiving, however, the family, which includes Tim’s wife, Trista, and their 8-year-old son and 11-year-old daughter, could tell Milo was feeling out of sorts.
“We noticed he was limping around a bit and being really lethargic,” says Gordon. At first they attributed his behavior to the influx of guests they had around the holiday. Then they started to worry about hip dysplasia. But in early December, Gordon’s 8-year-old son noticed a bulge in Milo’s leg near his paw.
The family brought their pet to the veterinarian expecting to learn he had a sprain or even a broken bone, but a graver diagnosis came back: osteosarcoma. Wanting to participate in a clinical trial, the family made several trips to Penn Vet from their home near Baltimore to get him evaluated and then for the radiation, limb removal surgery, and follow up.
Not only did participating in the clinical trial help the Gordons cover some of the costs of treatment, but they also appreciated the opportunity to contribute to studies that may advance cancer treatment.
“That kept us going,” says Trista Gordon. “Even my daughter kept saying that Milo could help other dogs or even children who have this disease. That eased her sadness in a way.”
That was especially resonant since Tim Gordon lost his mother to osteosarcoma. “I knew what we went through with my mom and what she went through,” he says. “The thought definitely went through our minds that maybe we can help benefit other families by participating.”
Advancing medicine
The goal of radiation therapy, like all cancer-killing strategies, is to unleash a strong assault on tumor cells while sparing normal cells as much as possible. And while researchers have tweaked other facets of radiation, such as how it is aimed and how the dose is fractionated, or spread over days or weeks, it’s only very recently that the FLASH approach has opened the possibility of giving a full dose all at once.
Traditional radiation therapy uses the energy of photons, or X-rays, to kill cancer cells. Early work with FLASH radiation has used electrons to deliver that energy, but those can only penetrate tumors that are a few centimeters deep.
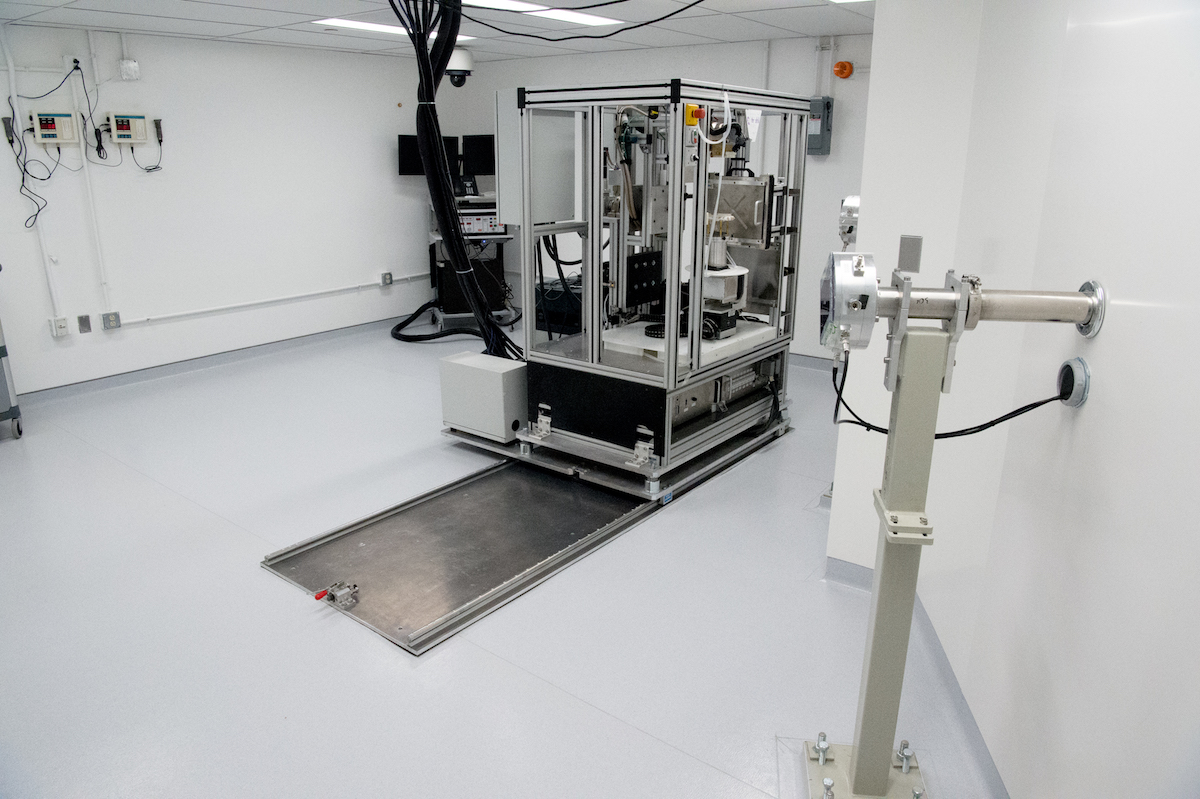
In January, Cengel and Penn Medicine colleagues including Constantinos Koumenis and James Metz reported on FLASH radiation using protons, which can penetrate deeper than electrons to allow treatment of the vast majority of human tumors by beaming in radiation from outside the body to target tumors and to spare normal tissues.