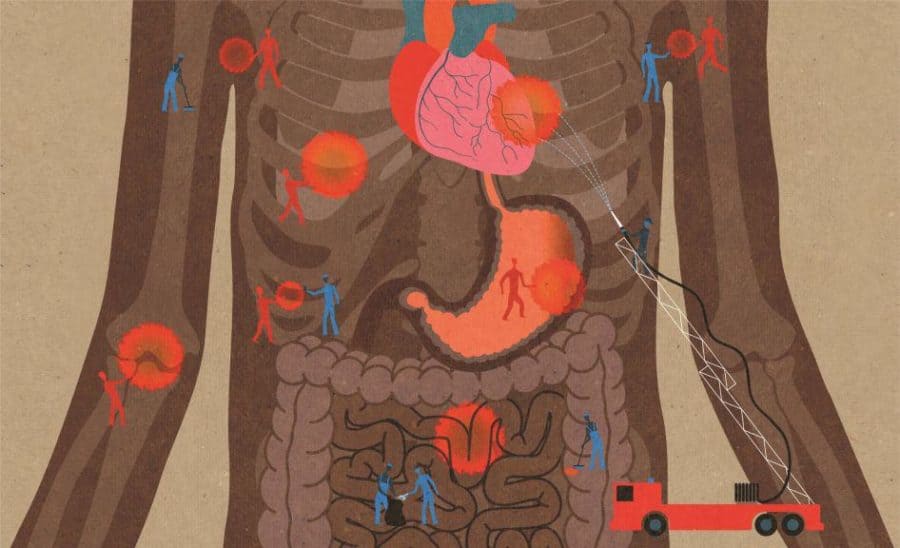
For many years, inflammation was considered one of medicine’s chief enemies. Experts viewed it as a side effect of illness and injury, a negative byproduct of the body’s efforts to heal. One managed and banished it whenever possible.
That view has undergone a major reassessment over the last decade. Inflammation, it turns out, isn’t always bad. In fact, researchers increasingly believe that it plays a vital role in maintaining good health. Some even believe inflammation is so central to the body’s proper functioning that our understanding of physiology must be rewritten.
“It (inflammation) is a very natural state,” said David A. Hafler, MD, the William S. and Lois Stiles Edgerly Professor of Neurology, professor of immunobiology, and chair of the School of Medicine’s Department of Neurology. “When you look at the immune system, it has multiple roles. The obvious one is fighting off infection. But the immune system has also been co-opted by nature to be used in a number of different systems for homeostasis. Inflammation is more than about just fighting off disease.”
Some examples: The immune system acts at times as a kind of cleanup crew that tidies up molecular messes. Elsewhere, it performs such functions totally unrelated to fighting microbes as pruning excess neurons in the brains of small children—an essential part of brain development. The immune system also helps regulate the function of many organs, including the liver and intestines. In doing all of these good things, it inevitably leaves residual inflammation.
A two-edged sword
While these insights recast inflammation as a more positive component of a person’s health, they also raise intriguing questions about how it may cause illness later in life. Are such diseases as cancer, for example, triggered when the immune system’s maintenance and regulatory duties go awry, often in connection with a gene, and cause too much inflammation?
“The immune system is a two-edged sword,” said John MacMicking, PhD, an associate professor of microbial pathogenesis and of immunobiology, and a Howard Hughes Medical Institute (HHMI) investigator. “Some things help protect you. Some things put you in harm’s way. Researchers are looking for the right balance.”
Inflammation has already been identified as a culprit instead of just a side effect in many illnesses, including multiple sclerosis (MS) and other autoimmune diseases. We have also learned that it plays a role in so-called lifestyle illnesses and such conditions as heart disease, obesity, and diabetes, said Akiko Iwasaki, PhD, the Waldemar Von Zedtwitz Professor of Immunobiology, professor of molecular, cellular and developmental biology, and an HHMI investigator. It’s hard to think of any disease that does not involve inflammation, Iwasaki said. That fact has some researchers calling for a wholesale reassessment of inflammation’s role in the body’s functioning.
“We still think in terms of normal physiology and abnormal inflammation,” said the Sterling Professor of Immunobiology and HHMI investigator Ruslan Medzhitov, PhD, one of the world’s leading inflammation researchers. “That view is, I think, outdated. There’s no modern framework to replace that view.”
Medzhitov and his lab are hard at work building that scaffolding. He argues that inflammation is as central to understanding physiology as are hormones. Once the initial work is complete, the next stage will be to try to find ways to turn inflammation on and off to treat or forestall disease, he said. He estimates we are about halfway to mapping the basics but only 10% of the way toward fully understanding how inflammation works.
“It’s clear that inflammation is not just about infection,” he said. “It’s not just a response to injury. It has multiple other job descriptions, multiple other functions that are involved also in what we call normal physiology.”
In a pioneering step, the medical school has incorporated Medzhitov’s findings into its curriculum, teaching future doctors that inflammation is an integral part of both health and sickness, not simply a side effect. As research attaches ever greater importance to inflammation, Yale is considering the establishment of an institute devoted exclusively to its study, according to Medzhitov and other researchers at the school. Understanding the role of inflammation in the body at the molecular level could pave the way for a new generation of pharmaceuticals and treatments. Because inflammation accompanies nearly every illness and disease, the potential for new developments is enormous.
“If you are infected, inflammation can even be a good thing, helping provide additional signals that alert the host to the presence of microbial pathogens and recruiting immune cells to the site of infection. However, you need to turn it off once the infection is resolved to avoid excessive tissue damage,” MacMicking said. “Is there a way to do that? Can I take a pill that helps reduce the inflammatory burden?”
The role of cytokines
On a basic level, our understanding of inflammation hasn’t changed, Iwasaki said. Inflammation from a broken ankle or a bronchial illness, for example, is the body’s way of summoning the immune system to restore homeostasis. Too much inflammation in and of itself can kill by, for example, flooding the lungs with fluid or causing dehydration.
Now we understand that inflammation can be both a cause and an effect, Iwasaki said. Obesity and diabetes are examples, she continued. When people become overweight, their fat cells become bigger. Immune system cells called macrophages, whose job is to maintain homeostasis, sense something is wrong, and they deploy disease-fighting small proteins called cytokines against the cells, creating inflammation. While the tipping point remains unclear—it appears to vary from person to person—the resulting inflammation can lead to diabetes and heart disease. Exactly how that happens requires further study, said Iwasaki. “We just know that if we can block these macrophages from firing, we can prevent the disease from happening,” she said.
Another example is Alzheimer’s disease, Iwasaki said. Research indicates that an immune reaction to amyloid plaques in the brain may contribute to the dreaded illness. According to the model, macrophages interpret crystal-like plaques in the brain as foreign objects and begin secreting cytokines that attack them, which leads to inflammation and destruction of neurons culminating in dementia. Ultimately, inflammation may also play a role in such behaviors as depression and suicide, she said.
Hafler, an expert on MS, cites yet another example of the double duty performed by inflammatory cytokines. His lab compared spinal fluid from healthy medical students and patients with MS. Unsurprisingly, the fluid from MS patients was inflamed—but so was that of the healthy medical students. “We had a very hard time telling the difference between MS spinal fluid and normal spinal fluid,” he said. That’s because cytokines, in addition to fighting disease, also help regulate the nervous system in relation to synaptic connections, fluid absorption, and other functions, he said.
Keeping the microbiome healthy
There’s another potential source of sickness-inducing inflammation: the human gut. Researchers increasingly think that inflammation in the digestive tract may be the point of origin of a variety of diseases, including neurodegenerative illnesses like Parkinson’s. They are also coming to believe that a healthy microbiome—the billions of bacteria in the gut that help us process food—may be key to avoiding that potentially disease-inducing inflammation.
Noah Palm, PhD ’11, FW ’15, assistant professor of immunobiology, and his lab team are probing the connections between the microbiome, inflammation, and disease. The microbiome is exquisitely sensitive, Palm said. Changes in diet, or even something as seemingly benign as living with a dog, significantly alter the teeming microbial communities that populate our guts, he said. As the Western environment has become more antiseptic and most people’s diets contain fewer plants and more processed foods, the makeup of our gut microbiome has changed, and its diversity has declined significantly. At the same time, the incidence of certain inflammatory illnesses and conditions—allergies, obesity, heart disease, diabetes—has exploded. Is there a connection?
“In my lab, we are trying to make the transition from correlation to causation,” said Palm. He has already begun to establish potential causation in certain illnesses, specifically inflammatory bowel disease (IBD). He and his lab assistants have found that when microbiome material from an IBD sufferer is inserted into an otherwise healthy mouse, the mouse will develop a disease that looks similar to human IBD. While genetic factors may also be involved, these findings indicate that particular bacteria may trigger IBD in at least a subset of patients. Palm’s research has a long way to go, but it could ultimately lead to individualized treatments designed to maximize microbiome health and stave off disease-inducing inflammation.
A new approach to antibiotic resistance
The expanded understanding of inflammation in the gut and how it is induced could also one day address one of medicine’s biggest long-term challenges: antibiotic resistance. Jorge Galán, PhD, DVM, the Lucille P. Markey Professor of Microbial Pathogenesis, professor of cell biology, and chair of the Department of Microbial Pathogenesis, said his lab studies “in detail” intestinal tract diseases—especially salmonellosis. The long-held view was that the inflammation resulting from Salmonella infection, which makes you sick, was caused by the immune system’s attacking the pathogen. But “we now know that this is not the case,” Galán said.
Nutrients are scarce in the gut, Galán added. In order to make those nutrients available, Salmonella and similar pathogens must induce inflammation. That’s not easy because the immune system is tamped down in the gut; otherwise recognition of the bacteria in the microbiome would trigger a chronic state of inflammation. “Salmonella needs inflammation,” Galán said. “Its stomping ground is the gut. Now it’s got a problem. It needs inflammation in a place where it’s not easy to trigger it.”
Salmonella meets this goal by injecting proteins that trigger inflammation, thereby producing the nutrients it needs to survive, Galán said. He has on a table in his office a clear block containing an image of the pathogen’s microinjection device, a gift from his students. Most of the time, the resulting inflammation isn’t enough to make a person sick because the pathogen uses its own mechanisms to turn it off; it’s when inflammation gets out of control, which is rare, that one develops the classic symptoms of salmonellosis. “That is what is so cool about inflammation,” Galán said. “There are so many ways to trigger it.”
Galán’s insight potentially creates a new treatment pathway. Instead of killing the pathogen with a classic antibiotic, you can try to formulate a targeted drug that simply shuts off the microinjection device inducing the inflammation, he said. “You gum up the bacteria,” Galán said. “You are preventing the bacteria from causing disease, which is a totally different concept. Certainly the evolutionary process that leads to antibiotic resistance would be slowed significantly.”
The promise of a deeper understanding of inflammation and its roles in sickness and health is significant, potentially paving the way for individualized and less invasive treatments that work in harmony with the body, researchers say. It may well boil down to learning how to turn inflammation from on to off.
“Can we uncouple the beneficial from the harmful effects?” MacMicking said. “Find new molecular targets that mount effective antimicrobial responses but avoid the non-collateral damage. Cytokine signaling turns on hundreds of genes—is there a way to pick and choose downstream host responses we’d like to elicit and quieten those we wish to avoid?” MacMicking and his fellow Yale researchers are working to find out.