Researchers at The Ohio State University College of Medicine are the first to identify an immune cell that may predict a transplant patient’s risk of developing antibodies that can cause organ rejection. This discovery could lead to the development of therapies to prevent complications after transplant surgery.
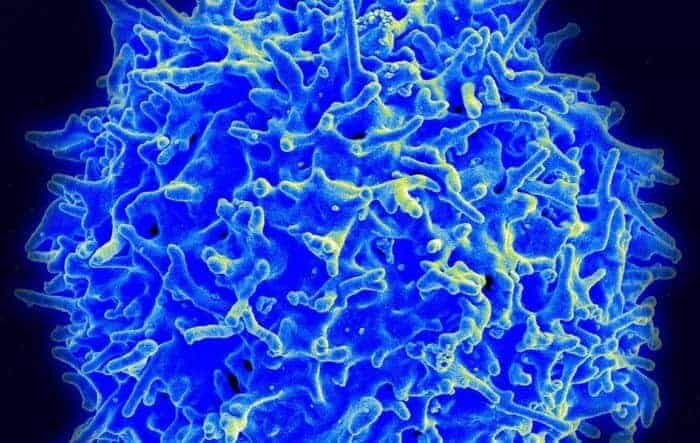
“Donor-specific antibodies (DSA) can cause immediate damage to the transplanted organ, known as acute rejection, or over time can lead to chronic organ rejection,” said Dr. Ginny Bumgardner, associate dean of research education and professor of surgery at the College of Medicine and transplant surgeon at The Ohio State University Wexner Medical Center. “The CD8+ T immune cell subset we discovered has the capacity to reduce antibody production in transplant recipients.”
The study, published in the journal Transplantation, followed 95 first-time kidney transplant patients for one year post-transplant. The patients were monitored for the development of DSA pre-transplant and at 1, 3, 6, 9 and 12 months after transplant. All of the patients were DSA-negative before transplant and received standard immunosuppression therapy after surgery.
Nearly 25% of the patients in the study developed DSA. There were no significant differences between the DSA-positive and DSA-negative patients in the primary cause of kidney disease, donor type (living or deceased) or length of dialysis prior to transplant. However, the DSA-positive patients had significantly lower quantities of a particular subset of CD8+ T cells compared to the patients that remained DSA-negative over the first year after transplant.
“Not only was one year rejection-free and overall graft survival lower in DSA-positive patients compared to DSA-negative patients, the development of DSA was associated with higher hospital readmissions, higher rates of infection and higher rates of acute rejection,” Bumgardner said.
Future research will focus on strategies to monitor recipient CD8+T cells to predict the risk of developing DSA so doctors can identify patients who could benefit from higher target levels of immunosuppression to prevent the development of DSA, or more frequent monitoring for DSA to diagnose acute organ rejection at an earlier stage. The research team is also exploring using CD8+ T cells to create treatment options before and after surgery.
In 2019, 39,719 transplant surgeries were performed in the United States. With more than 110,000 Americans waiting for a transplant, this research may help increase the number of first time transplant surgeries by reducing the number of recipients who experience acute rejection of their transplanted organ and need for a second transplant surgery.
“We could potentially use these cells as a therapy to do two things,” Bumgardner said. “One to prevent antibody development in the first place, antibodies that are directed against the donor organ. And second, for patients who do develop antibody mediated rejection, we may be able to use the cells as a therapy to suppress ongoing antibody production and stop the rejection.”