Researchers at UC San Francisco have developed a “digital biomarker” that would use a smartphone’s built-in camera to detect Type 2 diabetes – one of the world’s top causes of disease and death – potentially providing a low-cost, in-home alternative to blood draws and clinic-based screening tools.
Type 2 diabetes affects more than 32 million Americans and more than 450 million people worldwide, and can raise the risk of diseases affecting nearly every organ system, including coronary heart disease, kidney failure, blindness and stroke. In the current pandemic, it also has been found to increase the risk of severe symptoms of COVID-19.
Yet, half of the people with diabetes are unaware of their diagnosis and risks to their health.
“The ability to detect a condition like diabetes that has so many severe health consequences using a painless, smartphone-based test raises so many possibilities,” said co-senior author Geoffrey H. Tison, MD, MPH, assistant professor in cardiology, of the Aug. 17, 2020, study in Nature Medicine. “The vision would be for a tool like this to assist in identifying people at higher risk of having diabetes, ultimately helping to decrease the prevalence of undiagnosed diabetes.”
Screening tools that can be deployed easily, using technology already contained in smartphones, could rapidly increase the ability to detect diabetes, the researchers said, including populations out of reach of traditional medical care.
While diabetes mellitus is the seventh highest global cause of death on its own, according to the World Health Organization, it also significantly raises the risk of heart disease, which is the leading cause of death in the United States and worldwide. The U.S. Centers for Disease Control and Prevention estimate that people with Type 2 diabetes are twice as likely to die of heart disease as those who do not have diabetes.
“Diabetes can be asymptomatic for a long period of time, making it much harder to diagnose,” said lead author Robert Avram, MD, MSc, clinical instructor in cardiology. “To date, noninvasive and widely-scalable tools to detect diabetes have been lacking, motivating us to develop this algorithm.”
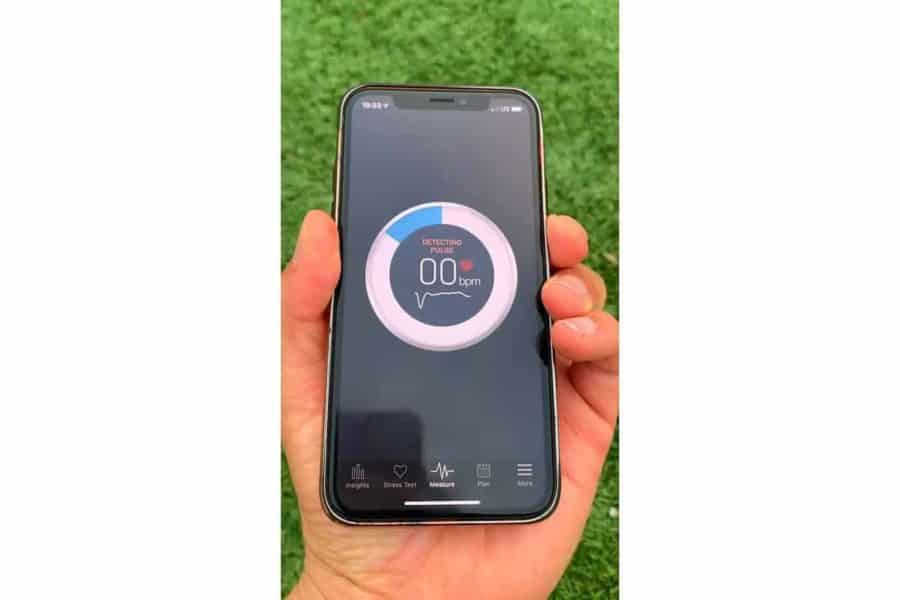
In developing the biomarker, the researchers hypothesized that a smartphone camera could be used to detect vascular damage due to diabetes by measuring signals called photoplethysmography (PPG), which most mobile devices, including smartwatches and fitness trackers, are capable of acquiring. The researchers used the phone flashlight and camera to measure PPGs by capturing color changes in the fingertip corresponding with each heartbeat.
In the Nature Medicine study, UCSF researchers obtained nearly 3 million PPG recordings from 53,870 patients in the Health eHeart Study who used the Azumio Instant Heart Rate app on the iPhone and reported having been diagnosed with diabetes by a health care provider. This data was used to both develop and validate a deep-learning algorithm to detect the presence of diabetes using smartphone-measured PPG signals.
Overall, the algorithm correctly identified the presence of diabetes in up to 81 percent of patients in two separate datasets. When the algorithm was tested in an additional dataset of patients enrolled from in-person clinics, it correctly identified 82 percent of patients with diabetes.
Among the patients that the algorithm predicted did not have diabetes, 92 to 97 percent indeed did not have the disease across the validation datasets. When this PPG-derived prediction was combined with other easily obtainable patient information, such as age, gender, body mass index and race/ethnicity, predictive performance improved further.
At this level of predictive performance, the authors said the algorithm could serve a similar role to other widespread disease screening tools to reach a much broader group of people, followed by a physician’s confirmation of the diabetes diagnosis and a treatment plan.
“We demonstrated that the algorithm’s performance is comparable to other commonly used tests, such as mammography for breast cancer or cervical cytology for cervical cancer, and its painlessness makes it attractive for repeated testing,” said study author Jeffrey Olgin, MD, a UCSF Health cardiologist and professor and chief of the UCSF Division of Cardiology. “A widely accessible smartphone-based tool like this could be used to identify and encourage individuals at higher risk of having prevalent diabetes to seek medical care and obtain a low-cost confirmatory test.”
The authors recommend further study to determine the effectiveness of this approach for specific clinical applications, such as screening or therapeutic monitoring.
Co-Authors: Co-senior author Kirsten Aschbacher, PhD, Gregory Marcus, MD, MAS, and Mark Pletcher, MD, MPH, of UCSF; J. Weston Hughes, of UC Berkeley; and Peter Kuhar, of Azumio Inc.
Funding: Avram received support from the Fonds de la recherche en santé du Québec (grant 274831). Tison, Olgin, Pletcher and Marcus received support from the National Institutes of Health (NHLBI K23HL135274, U2CEB021881). Pletcher is partially supported by a Patient-Centered Outcomes Research Institute contract supporting the Health eHeart Alliance (PPRN-1306-04709).
Disclosures: Olgin has received research funding from Samsung and iBeat. Marcus has received research funding from Medtronic, Jawbone and Eight. Aschbacher received funding from Jawbone Health Hub. Tison has received research grants from Janssen Pharmaceuticals and Myokardia and is an advisor to Cardiogram, Inc. Azumio provided no financial support for this study and only provided access to data.